Ophthalmic Technology: Revolutionizing Eye Care
Opthalmic technology – Ophthalmic technology has revolutionized the way we diagnose, treat, and manage eye conditions. From the invention of the ophthalmoscope to the development of artificial intelligence-powered tools, technological […]

Opthalmic technology – Ophthalmic technology has revolutionized the way we diagnose, treat, and manage eye conditions. From the invention of the ophthalmoscope to the development of artificial intelligence-powered tools, technological advancements have significantly improved patient outcomes and expanded access to eye care services.
This journey through ophthalmic technology explores the evolution of diagnostic tools, surgical procedures, therapeutic devices, and emerging technologies. We delve into the principles behind these innovations, their impact on clinical practice, and their potential to shape the future of eye care.
Evolution of Ophthalmic Technology: Opthalmic Technology
The field of ophthalmic technology has undergone a remarkable transformation, driven by continuous advancements that have revolutionized the way we diagnose, treat, and manage eye conditions. From the invention of the first eyeglasses to the advent of laser surgery and artificial vision, the journey of ophthalmic technology has been marked by groundbreaking innovations that have significantly improved patient care and vision outcomes.
Historical Advancements in Ophthalmic Technology
The evolution of ophthalmic technology is a testament to human ingenuity and the relentless pursuit of improving vision. Key breakthroughs have paved the way for modern eye care practices, shaping the field as we know it today.
- Early Eyeglasses: The invention of eyeglasses in the 13th century marked a pivotal moment in ophthalmic history. These early lenses, crafted from glass or quartz, provided the first means of correcting refractive errors, allowing people with vision impairments to see more clearly. This simple invention revolutionized the lives of millions and laid the foundation for future advancements in optics.
- The Ophthalmoscope: In the 19th century, the invention of the ophthalmoscope by Hermann von Helmholtz enabled physicians to visualize the interior of the eye for the first time. This breakthrough instrument allowed for the diagnosis and treatment of a wide range of eye diseases, ushering in a new era of understanding and care for the eye. The ophthalmoscope revolutionized eye care by allowing doctors to see inside the eye, enabling the diagnosis and treatment of conditions like diabetic retinopathy, macular degeneration, and glaucoma.
- Lasik Surgery: The development of LASIK (Laser-Assisted In Situ Keratomileusis) surgery in the late 20th century marked a significant leap forward in refractive surgery. This minimally invasive procedure uses a laser to reshape the cornea, correcting refractive errors like myopia, hyperopia, and astigmatism. LASIK surgery has provided millions of people with improved vision and reduced their dependence on eyeglasses or contact lenses.
Comparison of Traditional and Modern Techniques
Traditional methods in ophthalmology often relied on manual techniques and limited diagnostic tools. Modern techniques, however, have been revolutionized by the integration of advanced technologies, offering significant advantages in terms of precision, accuracy, and patient comfort.
- Diagnosis: Traditional methods relied heavily on subjective assessments, such as visual acuity tests and patient descriptions of symptoms. Modern techniques utilize sophisticated imaging technologies, such as OCT (Optical Coherence Tomography) and fundus photography, to provide detailed, objective insights into the structure and function of the eye. These advanced imaging techniques have significantly improved diagnostic accuracy, allowing for early detection and intervention of eye diseases.
- Treatment: Traditional treatments often involved invasive procedures, such as cataract surgery using manual techniques. Modern techniques utilize minimally invasive procedures, such as phacoemulsification for cataract surgery and laser-based treatments for glaucoma, resulting in faster recovery times, reduced complications, and improved patient outcomes.
Impact of Technological Advancements on Eye Care
Technological advancements have played a pivotal role in improving diagnostic accuracy, treatment effectiveness, and patient outcomes in ophthalmology.
- Improved Diagnostic Accuracy: The integration of advanced imaging technologies, such as OCT and fundus photography, has significantly improved diagnostic accuracy. These technologies provide detailed, objective insights into the structure and function of the eye, enabling earlier detection and intervention of eye diseases. Early detection and treatment are crucial for preserving vision and preventing further damage.
- Enhanced Treatment Effectiveness: Modern techniques, such as laser-based treatments for glaucoma and phacoemulsification for cataract surgery, have significantly enhanced treatment effectiveness. These minimally invasive procedures offer faster recovery times, reduced complications, and improved patient outcomes.
- Personalized Eye Care: Technological advancements have enabled personalized eye care, allowing for tailored treatments based on individual patient needs. For example, advanced imaging technologies can provide detailed information about the structure and function of a patient’s eye, allowing for customized treatments and personalized management plans.
Diagnostic Tools and Techniques
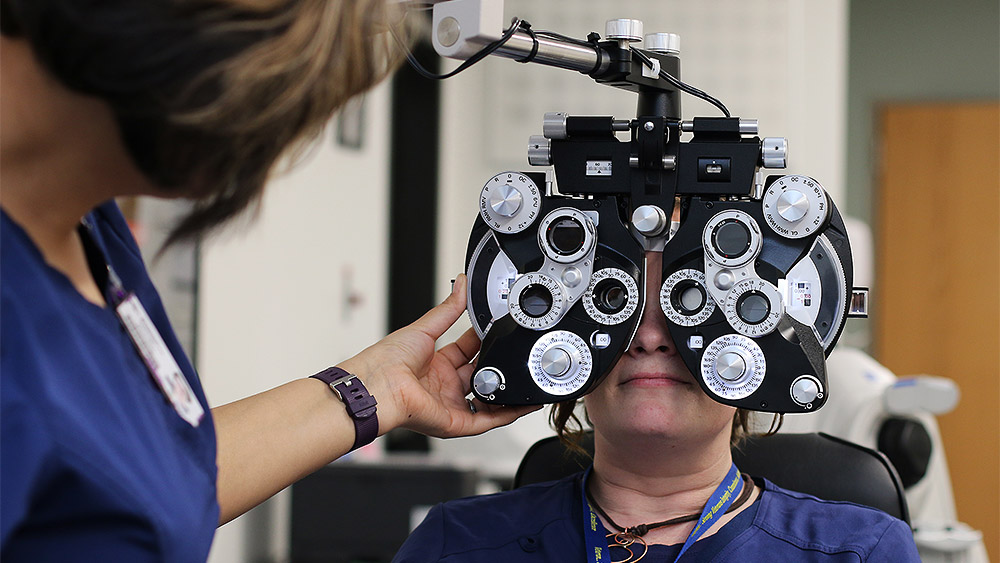
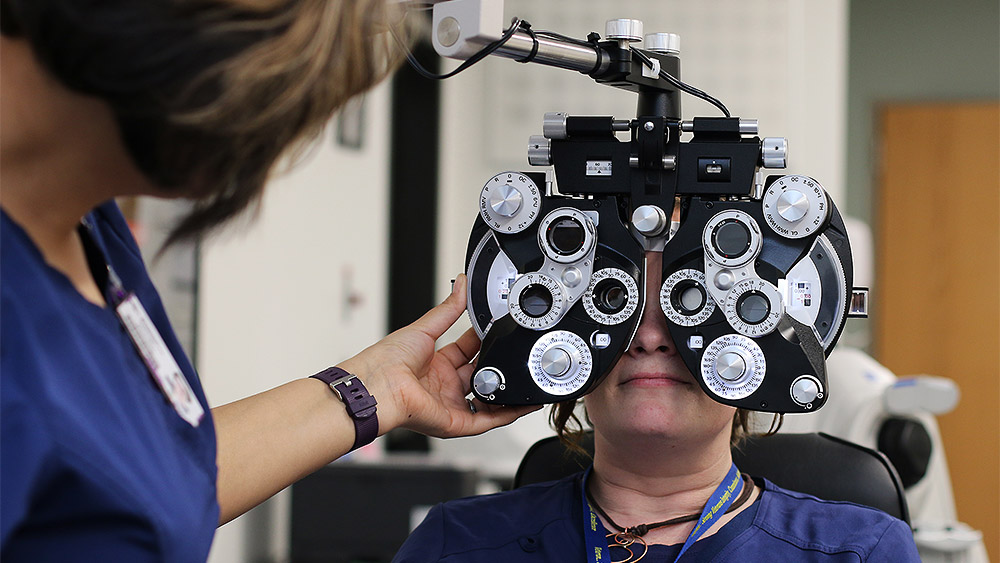
Ophthalmologists employ a range of diagnostic tools and techniques to thoroughly assess eye health and identify underlying conditions. These tools allow for precise examination of the eye’s internal structures, enabling early detection and effective management of various eye diseases.
Ophthalmoscope
The ophthalmoscope is an essential tool for examining the interior of the eye, specifically the retina, optic nerve, and blood vessels. It illuminates the eye’s interior and magnifies the view, allowing the ophthalmologist to visualize potential abnormalities.
Types of Ophthalmoscopes
- Direct ophthalmoscope: This handheld device provides a magnified, upright, and virtual image of the fundus. It is widely used for routine eye examinations.
- Indirect ophthalmoscope: This type uses a lens system to project an inverted, real image of the fundus onto a screen. It offers a wider field of view and is often used for detailed examination of the peripheral retina.
Principles of Operation
The ophthalmoscope utilizes a light source and a lens system to project light into the eye and magnify the reflected image. The light source illuminates the eye’s interior, while the lens system focuses the reflected light onto the observer’s eye.
Role in Diagnosis
The ophthalmoscope plays a crucial role in diagnosing various eye conditions, including:
- Diabetic retinopathy: This condition damages blood vessels in the retina, leading to vision loss. The ophthalmoscope helps identify signs of damage, such as microaneurysms, hemorrhages, and exudates.
- Glaucoma: This condition damages the optic nerve, leading to vision loss. The ophthalmoscope allows visualization of the optic nerve head, enabling assessment for any signs of damage.
- Macular degeneration: This condition affects the central part of the retina, leading to vision loss. The ophthalmoscope helps identify signs of macular degeneration, such as drusen, pigment changes, and retinal detachment.
Tonometer, Opthalmic technology
The tonometer is a specialized instrument used to measure the intraocular pressure (IOP), which is the pressure inside the eye. IOP is an important indicator of eye health, as elevated IOP can be a sign of glaucoma.
Types of Tonometers
- Applanation tonometer: This type uses a small, flat probe to flatten the cornea, measuring the force required to achieve a specific degree of flattening. This force is then used to calculate the IOP.
- Non-contact tonometer (NCT): This type uses a puff of air to flatten the cornea, measuring the pressure required to achieve a specific degree of flattening. This method is non-invasive and less likely to cause discomfort.
Principles of Operation
The applanation tonometer relies on the principle of Imbert-Fick law, which states that the force required to flatten a curved surface is proportional to the pressure inside the surface. The NCT uses a similar principle, but instead of a probe, it uses a puff of air to flatten the cornea.
Role in Diagnosis
The tonometer is crucial for diagnosing and monitoring glaucoma. Elevated IOP is a major risk factor for glaucoma, and regular IOP measurements help ophthalmologists detect early signs of the disease and initiate appropriate treatment.
Optical Coherence Tomography (OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique that provides high-resolution cross-sectional images of the retina and optic nerve. It uses light waves to create detailed images of the eye’s internal structures, allowing ophthalmologists to identify subtle changes that may not be visible with other techniques.
Types of OCT
- Spectral-domain OCT (SD-OCT): This type uses a broad spectrum of light to create images, offering faster scanning speeds and improved image quality compared to time-domain OCT.
- Swept-source OCT (SS-OCT): This type uses a tunable laser to create images, providing even faster scanning speeds and deeper penetration into the eye.
Principles of Operation
OCT works by measuring the time it takes for light waves to reflect back from different layers of the eye. By analyzing the reflected light, the OCT machine creates a detailed, three-dimensional image of the eye’s internal structures.
Role in Diagnosis
OCT is a valuable tool for diagnosing and monitoring various eye conditions, including:
- Macular degeneration: OCT can identify subtle changes in the macula, such as drusen, fluid buildup, and retinal thinning, which may not be visible with other techniques.
- Diabetic retinopathy: OCT can detect early signs of diabetic retinopathy, such as microaneurysms, hemorrhages, and retinal thickening.
- Glaucoma: OCT can assess the optic nerve head, measuring the thickness of the retinal nerve fiber layer, which can be affected by glaucoma.
Other Diagnostic Tools
- Slit lamp: This instrument uses a narrow beam of light to examine the anterior segment of the eye, including the cornea, iris, lens, and anterior chamber. It allows for detailed visualization of these structures and identification of abnormalities.
- Visual field analyzer: This device measures the peripheral vision, detecting areas of vision loss that may be caused by glaucoma or other conditions affecting the optic nerve.
- Fundus camera: This instrument captures high-resolution images of the retina, allowing for detailed documentation and analysis of any abnormalities.
Surgical Interventions and Procedures
Ophthalmic surgery encompasses a wide range of procedures designed to address various eye conditions, from refractive errors to complex retinal diseases. These interventions often involve meticulous techniques and advanced technologies, aiming to restore vision and improve patients’ quality of life.
Cataract Surgery
Cataract surgery is one of the most common ophthalmic procedures, involving the removal of the clouded natural lens and its replacement with an artificial intraocular lens (IOL). This procedure is typically performed on an outpatient basis, with a high success rate.
The evolution of cataract surgery has been marked by significant advancements, transitioning from traditional techniques to minimally invasive approaches. The introduction of phacoemulsification, a technique that uses ultrasound waves to break up the cataract, revolutionized the procedure, making it less invasive and improving recovery time.
Modern cataract surgery often employs femtosecond lasers to create precise incisions and break up the cataract, further enhancing accuracy and minimizing complications.
LASIK
LASIK (Laser-Assisted In Situ Keratomileusis) is a refractive surgery procedure that reshapes the cornea to correct vision problems such as myopia, hyperopia, and astigmatism. This procedure is performed using a specialized laser to create a thin flap in the cornea, which is then lifted and reshaped by the laser.
The evolution of LASIK has witnessed advancements in laser technology, resulting in faster and more precise treatments. The use of wavefront technology allows for personalized treatments based on individual eye characteristics, further enhancing outcomes.
Retinal Detachment Repair
Retinal detachment occurs when the retina, the light-sensitive tissue at the back of the eye, detaches from its underlying layer. This condition can lead to significant vision loss if left untreated. Retinal detachment repair aims to reattach the retina to its proper position.
Surgical techniques for retinal detachment repair vary depending on the severity and location of the detachment. Common procedures include scleral buckling, vitrectomy, and pneumatic retinopexy.
Scleral buckling involves placing a silicone band around the eye to compress the sclera (the white part of the eye), pushing the retina back into place. Vitrectomy involves removing the vitreous humor, the gel-like substance that fills the eye, and replacing it with a gas or oil bubble to hold the retina in place. Pneumatic retinopexy involves injecting a gas bubble into the eye to push the retina back into place.
Technological advancements in microscopes, lasers, and surgical instruments have significantly improved the precision and effectiveness of retinal detachment repair procedures.
Therapeutic Devices and Treatments

Ophthalmic therapeutic devices play a crucial role in managing and treating various eye conditions. These devices, ranging from intraocular lenses to drug delivery systems, aim to restore vision, improve eye health, and enhance patient quality of life. This section explores the different types of therapeutic devices, their mechanisms of action, and their effectiveness in addressing specific eye conditions.
Intraocular Lenses
Intraocular lenses (IOLs) are artificial lenses implanted within the eye to replace the natural lens, which may have been removed due to cataract surgery or other eye conditions. IOLs are designed to restore clear vision and reduce the need for glasses or contact lenses.
- Types of IOLs:
- Monofocal IOLs: Provide clear vision at a single distance, typically for distance vision. These are the most common type of IOLs.
- Multifocal IOLs: Designed to provide clear vision at multiple distances, including near, intermediate, and far. They offer the potential for reduced dependence on glasses.
- Toric IOLs: Correct astigmatism, a common refractive error that causes blurry vision. These IOLs have a specific shape to compensate for the irregular curvature of the cornea.
- Accommodative IOLs: Designed to mimic the natural focusing ability of the eye, allowing for near and far vision without the need for glasses.
- Mechanism of Action: IOLs function by refracting light rays onto the retina, similar to the natural lens. They are surgically placed within the eye’s capsular bag, which holds the natural lens.
- Effectiveness: IOLs are highly effective in restoring vision after cataract surgery or other lens-related eye conditions. They have a high success rate, with most patients achieving excellent visual acuity.
Contact Lenses
Contact lenses are small, curved lenses worn directly on the eye’s surface to correct refractive errors and improve vision. They offer a more discreet alternative to eyeglasses and are available in various materials and designs.
- Types of Contact Lenses:
- Soft Contact Lenses: Made from flexible materials that conform to the shape of the cornea. They are comfortable to wear and are suitable for most people.
- Rigid Gas Permeable (RGP) Lenses: Made from rigid, oxygen-permeable materials that provide sharper vision than soft lenses. They are typically used for individuals with astigmatism or other corneal irregularities.
- Disposable Contact Lenses: Designed for single-use or short-term wear. They are convenient and reduce the risk of eye infections.
- Specialty Contact Lenses: Developed for specific eye conditions, such as keratoconus or dry eye disease. They provide customized solutions to address unique vision needs.
- Mechanism of Action: Contact lenses work by refracting light rays before they reach the cornea, correcting refractive errors such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism.
- Effectiveness: Contact lenses are highly effective in improving vision for millions of people worldwide. They provide clear vision and allow for greater freedom of movement compared to eyeglasses.
Drug Delivery Systems
Drug delivery systems in ophthalmology are designed to deliver medications directly to the eye, maximizing therapeutic efficacy and minimizing systemic side effects. These systems offer various approaches to drug administration, each with its unique advantages and limitations.
- Types of Drug Delivery Systems:
- Eye Drops: The most common method of drug delivery, involving the instillation of liquid medication into the conjunctival sac. While convenient, eye drops have limited bioavailability due to rapid drainage and tear film dilution.
- Ointments: Provide sustained drug release compared to eye drops but can cause blurred vision and discomfort.
- Intravitreal Injections: Involve injecting medication directly into the vitreous humor, the gel-like substance filling the eye’s posterior chamber. This method allows for higher drug concentrations and longer duration of action but requires a sterile procedure and can be associated with potential complications.
- Sustained-Release Implants: Small, biocompatible implants placed in the eye to release medication over an extended period. They offer a convenient and long-acting drug delivery option, but require surgical implantation and may have potential risks.
- Drug-Eluting Contact Lenses: Contact lenses impregnated with medication that is released gradually into the eye. They offer a convenient and targeted drug delivery method, but require careful monitoring and may have limited drug capacity.
- Mechanism of Action: Drug delivery systems aim to achieve therapeutic concentrations of medication in the target tissue, whether it’s the cornea, conjunctiva, retina, or other ocular structures. The specific mechanism of action depends on the drug being delivered and the intended therapeutic effect.
- Effectiveness: Drug delivery systems have significantly improved the management of various eye conditions, including glaucoma, macular degeneration, and dry eye disease. They have increased treatment options and improved patient outcomes.
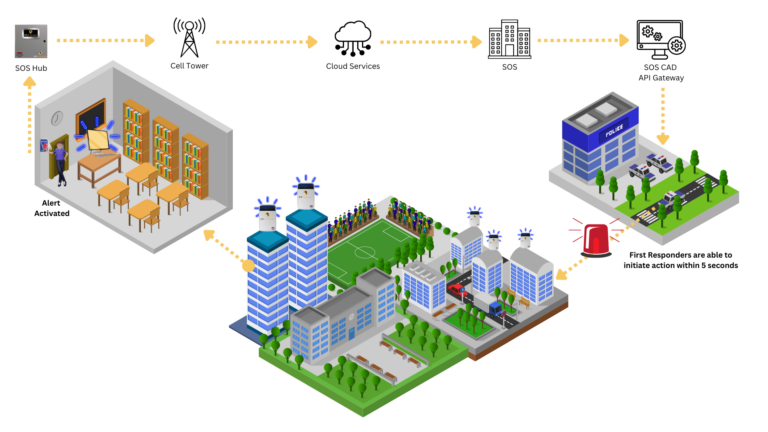
Teleophthalmology and Remote Monitoring
Teleophthalmology, the use of telecommunications technology to provide eye care services remotely, has emerged as a transformative force in ophthalmology, particularly in addressing the challenge of expanding access to eye care in underserved areas. This technology leverages the power of telemedicine platforms to enable remote diagnosis, consultation, and monitoring of eye conditions, bridging geographical gaps and improving patient outcomes.
The Role of Teleophthalmology in Expanding Access to Eye Care
Teleophthalmology plays a crucial role in expanding access to eye care services, particularly in underserved areas, by addressing the challenges of limited access to ophthalmologists and specialists. This technology facilitates remote diagnosis, consultation, and monitoring, enabling patients in remote locations to receive quality eye care without the need for extensive travel.
- Teleophthalmology allows for the delivery of eye care services to patients in rural and underserved communities, where access to specialists is limited. This is especially important in developing countries where healthcare infrastructure is often inadequate.
- Teleophthalmology can help to reduce the burden on healthcare systems by providing an alternative to traditional in-person consultations, particularly for routine check-ups and follow-up appointments.
- Teleophthalmology can also be used to provide specialized care to patients with rare or complex eye conditions, enabling them to access the expertise of specialists without having to travel long distances.
Telemedicine Platforms for Remote Eye Care
Telemedicine platforms have become essential tools for teleophthalmology, facilitating remote diagnosis, consultation, and monitoring of eye conditions. These platforms enable secure communication and data sharing between patients and healthcare providers, allowing for real-time interaction and collaboration.
- These platforms often incorporate features such as secure video conferencing, image sharing, and electronic health record integration, allowing for comprehensive remote eye care.
- Telemedicine platforms can be used for a wide range of eye care services, including initial consultations, follow-up appointments, diagnosis, and treatment planning.
- Some platforms also offer features for remote monitoring of eye conditions, such as automated reminders for medication refills and follow-up appointments, as well as tools for patients to track their symptoms and progress.
Challenges and Opportunities in Teleophthalmology
While teleophthalmology offers significant benefits, it also presents challenges that need to be addressed to ensure its successful implementation and widespread adoption.
- Patient Privacy and Data Security: Ensuring patient privacy and data security is paramount in teleophthalmology. Secure communication channels, robust encryption protocols, and adherence to data privacy regulations are essential to protect sensitive patient information.
- Regulatory Compliance: Teleophthalmology practices must comply with relevant regulations and licensing requirements in different jurisdictions. Establishing clear guidelines and standards for teleophthalmology services can facilitate wider adoption and ensure quality care.
- Technical Infrastructure: Reliable internet connectivity and access to appropriate telemedicine technology are essential for effective teleophthalmology. Addressing infrastructure limitations, particularly in underserved areas, is crucial for expanding access to remote eye care.
- Reimbursement and Cost-Effectiveness: Ensuring adequate reimbursement for teleophthalmology services is essential for its sustainability. Demonstrating the cost-effectiveness of teleophthalmology compared to traditional in-person care can help secure reimbursement and encourage its adoption.
- Public Acceptance and Awareness: Public awareness and acceptance of teleophthalmology are crucial for its success. Educational campaigns and patient outreach programs can help to address concerns and promote the benefits of remote eye care.
Future Directions and Emerging Technologies

The field of ophthalmology is constantly evolving, driven by advancements in technology and scientific understanding. This progress has led to groundbreaking treatments for various eye conditions, but the quest for improved vision restoration and prevention of vision loss continues. Emerging technologies hold immense promise for transforming the future of ophthalmology. These advancements are not only focused on addressing existing challenges but also on exploring new possibilities for vision care.
Gene Therapy
Gene therapy has emerged as a revolutionary approach for treating genetic eye diseases. This innovative technique involves delivering therapeutic genes directly into the eye, aiming to correct or compensate for defective genes responsible for vision loss. Gene therapy has shown promising results in clinical trials for inherited retinal diseases such as Leber’s congenital amaurosis (LCA) and retinitis pigmentosa (RP).
- In LCA, gene therapy has been shown to improve vision in some patients by replacing the faulty gene responsible for the disease.
- Similarly, gene therapy trials for RP have demonstrated the potential to slow down or halt the progression of vision loss.
Stem Cell Therapy
Stem cell therapy is another promising area of research in ophthalmology. Stem cells possess the unique ability to differentiate into various cell types, including retinal cells. This characteristic makes them a potential source for regenerating damaged or diseased retinal tissue.
- Clinical trials are underway to investigate the use of stem cells for treating age-related macular degeneration (AMD), a leading cause of vision loss in older adults.
- Stem cell therapy also holds promise for restoring vision in patients with retinal detachment and other conditions that damage the retina.
Bioprinting
Bioprinting, a cutting-edge technology, involves using 3D printing techniques to create living tissues and organs. In ophthalmology, bioprinting has the potential to revolutionize the development of artificial corneas and other eye tissues.
- Bioprinted corneas could provide a viable alternative to corneal transplants, which are often limited by donor availability.
- Bioprinting could also be used to create personalized eye implants tailored to individual patients’ needs.
Final Summary
Ophthalmic technology continues to evolve at an unprecedented pace, promising a future where vision loss can be prevented, treated, and even reversed. The convergence of advanced imaging, artificial intelligence, and minimally invasive techniques offers a brighter outlook for patients, enabling them to live life to the fullest.
Ophthalmic technology has advanced significantly in recent years, with new innovations constantly emerging. This progress is driven by a focus on improving patient care and enhancing visual experiences. One interesting development is the integration of “bird brain technologies,” which leverage the remarkable visual capabilities of birds , to further refine ophthalmic devices and techniques.
This interdisciplinary approach holds exciting potential for advancing our understanding of vision and developing more effective solutions for eye health.