Newest Technology in Dental Implants: Transforming Smiles
Newest technology in dental implants sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the […]
Newest technology in dental implants sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. Dental implants have revolutionized the way we replace missing teeth, providing a stable and long-lasting solution. But the field of implant dentistry is constantly evolving, with groundbreaking innovations emerging that are transforming patient care.
This exploration delves into the cutting-edge advancements that are shaping the future of dental implants. From digital dentistry and advanced materials to minimally invasive techniques and emerging technologies, we’ll uncover the latest developments that are making implant treatment more efficient, predictable, and aesthetically pleasing.
Digital Dentistry and Implant Planning
Digital dentistry has revolutionized implant planning, allowing for more precise and predictable outcomes. By integrating advanced technologies like digital impressions and 3D imaging, dental professionals can create virtual models of the patient’s mouth, enabling comprehensive planning before surgery. This eliminates the need for traditional plaster models and significantly enhances accuracy and efficiency.
Benefits of CAD/CAM Technology in Implant Design and Fabrication
CAD/CAM technology, or computer-aided design and computer-aided manufacturing, plays a crucial role in implant design and fabrication. This technology allows dentists to create customized implants that perfectly fit the patient’s anatomy. The process involves designing the implant using specialized software, which then generates a digital blueprint for fabrication.
- Enhanced Precision: CAD/CAM technology enables precise implant design and fabrication, ensuring optimal fit and function.
- Minimally Invasive Procedures: Customized implants often require smaller incisions, leading to less pain and faster healing.
- Improved Aesthetics: CAD/CAM allows for the creation of implants that seamlessly blend with the surrounding teeth, enhancing the patient’s smile.
- Reduced Surgical Time: Pre-designed implants can be placed more quickly, reducing surgical time and minimizing patient discomfort.
Examples of Software for Implant Simulation and Surgical Planning
Several software programs are available for implant simulation and surgical planning, each offering unique features and functionalities.
- NobelClinician: This software allows dentists to plan implant placement, simulate surgical procedures, and visualize potential complications. It also provides guidance for prosthetic restoration.
- 3Shape Implant Studio: This software offers comprehensive implant planning tools, including 3D imaging, virtual surgery, and prosthetic design. It integrates with various scanners and milling machines.
- Straumann CoDiagnostiX: This software combines 3D imaging and virtual planning to create a personalized treatment plan for implant cases. It enables precise implant placement and prosthetic design.
Digital Workflows Streamline Implant Placement and Reduce Surgical Time
Digital workflows streamline the entire implant process, from initial planning to final restoration. Digital impressions, 3D imaging, and CAD/CAM technology enable efficient and accurate treatment planning.
- Digital Impressions: Digital impressions are taken using intraoral scanners, which capture precise 3D images of the patient’s mouth. This eliminates the need for traditional plaster impressions, reducing time and discomfort.
- 3D Imaging: 3D imaging, such as cone-beam computed tomography (CBCT), provides detailed anatomical information, allowing dentists to plan implant placement with greater accuracy.
- Virtual Surgery: Virtual surgery software allows dentists to simulate the entire implant procedure, including bone preparation, implant placement, and prosthetic restoration. This enables them to identify potential complications and plan the most efficient surgical approach.
Advanced Implant Materials
The evolution of dental implants has been marked by advancements in materials science, leading to the development of new materials with enhanced properties. These materials play a crucial role in determining the success and longevity of dental implants.
Properties of New Implant Materials
The choice of implant material is critical for optimal biocompatibility, osseointegration, and aesthetics. Titanium alloys, zirconia, and other advanced materials are widely used in dental implantology.
- Titanium Alloys: Titanium alloys, such as commercially pure titanium (CP Ti) and titanium-aluminum-vanadium (Ti-6Al-4V), are the most commonly used materials for dental implants. Their excellent biocompatibility, osseointegration, and corrosion resistance make them ideal for this application. Titanium alloys exhibit high tensile strength, which is essential for resisting the stresses associated with chewing and biting forces. They also have a low modulus of elasticity, similar to bone, which helps minimize stress shielding and promotes bone growth around the implant.
- Zirconia: Zirconia (ZrO2) is a ceramic material with exceptional strength, biocompatibility, and aesthetic properties. Its high biocompatibility and resistance to corrosion make it a suitable alternative to titanium alloys. Zirconia implants are particularly beneficial for patients with metal allergies or who require implants in highly visible areas, as they offer a natural tooth-like appearance.
Advantages and Disadvantages of Different Implant Materials
Each implant material possesses distinct advantages and disadvantages, influencing its suitability for specific clinical situations.
- Biocompatibility: Titanium alloys and zirconia are highly biocompatible materials, meaning they are well-tolerated by the body and do not elicit an adverse immune response. This is crucial for successful osseointegration and long-term implant stability.
- Osseointegration: Osseointegration refers to the direct bonding of bone to the implant surface. Titanium alloys have excellent osseointegration properties due to their surface characteristics and ability to promote bone cell attachment and growth. Zirconia, while biocompatible, may exhibit slightly slower osseointegration rates compared to titanium.
- Aesthetics: Zirconia implants offer superior aesthetics compared to titanium implants, as they can be customized to match the natural tooth color. This is particularly important for implants placed in visible areas, such as the front teeth. However, zirconia implants are more expensive than titanium implants.
Role of Surface Modifications and Coatings
Surface modifications and coatings play a crucial role in enhancing implant integration and improving clinical outcomes.
- Surface Roughness: Increasing the surface roughness of implants can enhance osseointegration by providing more surface area for bone cells to attach and grow. This can be achieved through various methods, such as sandblasting, acid etching, or using micro-structured surfaces.
- Surface Coatings: Coatings can be applied to implant surfaces to improve biocompatibility, osseointegration, and aesthetic properties. For example, hydroxyapatite (HA) coatings are commonly used to enhance bone bonding, while titanium dioxide (TiO2) coatings can improve aesthetic properties.
Future of Implant Materials
The field of implant materials is constantly evolving, with ongoing research focusing on developing innovative materials with enhanced properties.
- Bioresorbable Materials: Bioresorbable materials, such as polylactic acid (PLA) and polyglycolic acid (PGA), are gradually absorbed by the body over time, eliminating the need for implant removal. This is particularly beneficial for patients with limited bone density or who require temporary implants.
- Personalized Implants: Personalized implants are designed based on individual patient needs and anatomy. This allows for precise implant placement and improved functional and aesthetic outcomes. Advancements in 3D printing technology are facilitating the development of personalized implants with customized shapes, sizes, and surface characteristics.
Minimally Invasive Implant Techniques
Minimally invasive techniques have revolutionized dental implant surgery, offering patients a more comfortable and efficient experience. These techniques aim to reduce surgical trauma, minimize tissue disruption, and promote faster healing.
Flapless Implant Surgery
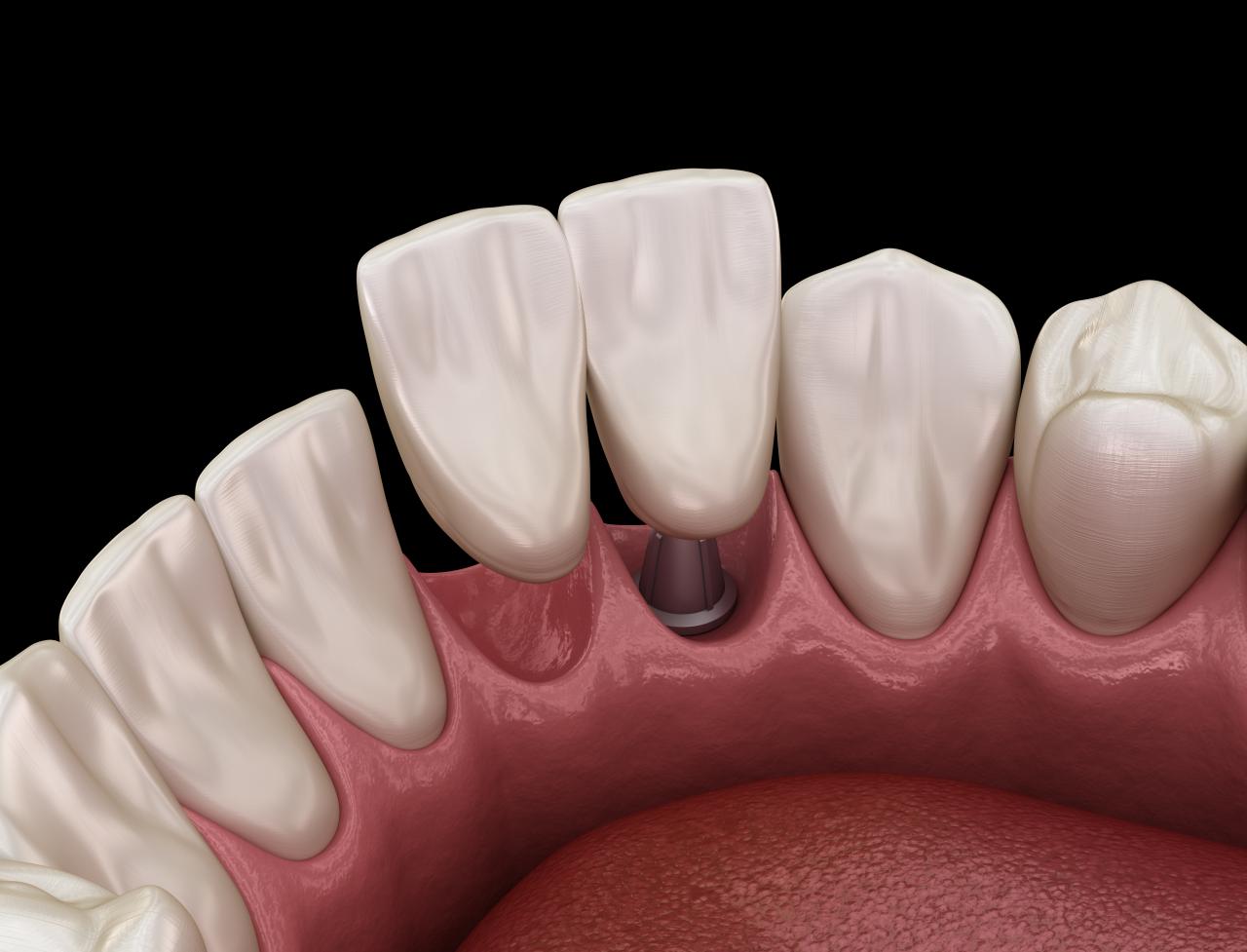
Flapless implant surgery, also known as minimally invasive implant surgery, is a technique that eliminates the need for a traditional surgical flap. Instead of cutting and lifting the gum tissue, a small incision is made in the gum, allowing the implant to be placed directly into the bone. This technique reduces postoperative pain, swelling, and discomfort, resulting in a faster recovery time.
Guided Implant Surgery
Guided implant surgery utilizes a 3D model of the patient’s jawbone, created from a CT scan, to plan and guide the placement of dental implants. This technique ensures precise implant placement, reducing the risk of nerve damage and improving implant stability. Guided surgery also minimizes the need for bone grafting, further reducing the invasiveness of the procedure.
Benefits of Minimally Invasive Implant Techniques
Minimally invasive techniques offer several benefits for patients, including:
- Reduced Pain and Discomfort: By minimizing tissue disruption, flapless techniques significantly reduce postoperative pain and swelling. Patients experience a faster recovery period with less discomfort.
- Faster Healing Time: The reduced trauma associated with minimally invasive techniques allows for faster tissue healing and a quicker return to normal activities.
- Improved Aesthetics: Flapless techniques minimize gum tissue damage, preserving the natural gum line and resulting in a more aesthetically pleasing outcome.
- Increased Precision and Accuracy: Guided surgery ensures precise implant placement, minimizing the risk of complications and maximizing the success rate of the procedure.
- Reduced Need for Bone Grafting: In some cases, guided surgery can eliminate the need for bone grafting, simplifying the procedure and reducing the overall treatment time.
Robotic-Assisted Implant Surgery, Newest technology in dental implants
Robotic-assisted implant surgery is a cutting-edge technology that utilizes robots to assist in the placement of dental implants. This technique offers even greater precision and accuracy than traditional guided surgery, minimizing human error and improving implant stability. The robot can also navigate complex anatomical structures, making it suitable for challenging cases.
Comparison of Traditional and Minimally Invasive Implant Techniques
| Feature | Traditional Implant Surgery | Minimally Invasive Implant Surgery |
|---|---|---|
| Surgical Flap | Required | Not required |
| Tissue Disruption | Significant | Minimal |
| Postoperative Pain and Swelling | Moderate to Severe | Minimal |
| Recovery Time | Longer | Shorter |
| Precision and Accuracy | Moderate | High |
| Aesthetics | May affect gum line | Preserves natural gum line |
Immediate Implant Placement and Loading
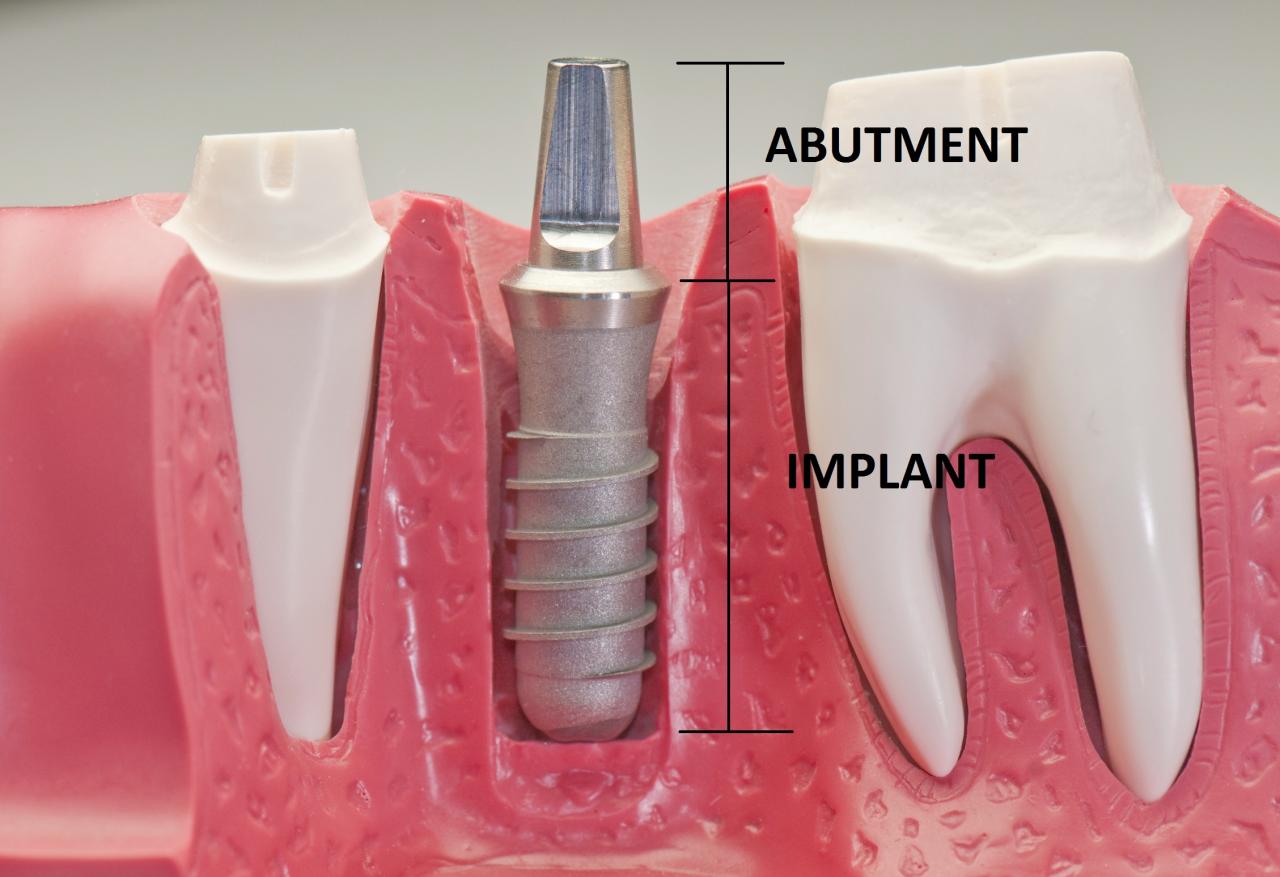
Immediate implant placement and loading is a dental procedure that involves placing an implant immediately after tooth extraction and restoring it with a temporary crown or prosthesis. This technique aims to shorten the treatment time and provide immediate esthetic and functional benefits to the patient.
Advantages and Disadvantages of Immediate Loading
Immediate loading offers several advantages compared to conventional implant protocols, which involve a healing period of several months before restoration.
- Reduced Treatment Time: Immediate loading eliminates the waiting period for bone healing, significantly reducing the overall treatment time.
- Improved Esthetics: Placing the implant immediately after extraction helps maintain the existing bone structure and minimizes bone resorption, contributing to better esthetics.
- Enhanced Function: Immediate restoration allows the patient to regain function sooner, improving their quality of life.
- Reduced Number of Surgical Procedures: Combining extraction and implant placement into a single procedure minimizes surgical interventions and potential complications.
However, immediate loading also has some disadvantages:
- Increased Risk of Implant Failure: Immediate loading can increase the risk of implant failure, especially in cases with compromised bone quality or inadequate implant stability.
- Higher Technical Demands: The procedure requires specialized skills and experience from the dentist to ensure proper implant placement and loading.
- Potential for Complications: Immediate loading can increase the risk of complications such as infection, peri-implantitis, and implant mobility.
- Limited Patient Selection: Not all patients are suitable candidates for immediate loading. Factors like bone quality, implant size, and patient compliance play a crucial role in determining suitability.
Factors Influencing the Success of Immediate Implant Placement
Several factors influence the success of immediate implant placement and loading.
- Bone Quality and Quantity: Adequate bone quality and quantity are essential for implant stability and long-term success.
- Implant Design and Size: The implant design and size should be carefully selected based on the patient’s anatomy and clinical requirements.
- Surgical Technique: Proper surgical technique, including meticulous tissue handling and precise implant placement, is crucial for successful immediate loading.
- Patient Compliance: Patient compliance with post-operative instructions, including meticulous oral hygiene and avoidance of excessive occlusal loading, is essential for healing and implant success.
- Occlusal Loading: The amount of force applied to the implant during chewing should be carefully controlled to prevent overloading and potential implant failure.
Steps Involved in Immediate Implant Placement and Loading
- Tooth Extraction: The affected tooth is extracted, ensuring proper bone preparation for implant placement.
- Implant Placement: The implant is immediately placed into the extraction socket, ensuring adequate primary stability.
- Temporary Restoration: A temporary crown or prosthesis is fabricated and placed over the implant, providing immediate function and esthetics.
- Healing and Osseointegration: The implant integrates with the surrounding bone tissue over time, typically within 3-6 months.
- Final Restoration: Once osseointegration is complete, the temporary restoration is replaced with a permanent crown or prosthesis.
Implant Supported Prostheses: Newest Technology In Dental Implants

Implant-supported prostheses have revolutionized dentistry, providing durable and aesthetically pleasing solutions for missing teeth. These prostheses, which are attached to dental implants, offer a wide range of benefits, including improved chewing function, enhanced speech clarity, and increased self-confidence.
Evolution of Implant-Supported Prostheses
The evolution of implant-supported prostheses has been driven by advancements in materials, designs, and aesthetics. Early implants were made from materials like titanium and were often bulky and noticeable. However, advancements in materials science have led to the development of biocompatible materials that are both strong and aesthetically pleasing.
- Improved Materials: The use of ceramic implants, such as zirconia, has gained popularity due to their excellent biocompatibility, high strength, and natural appearance. These materials mimic the color and translucency of natural teeth, resulting in highly aesthetic restorations.
- Enhanced Designs: Implant designs have evolved to be smaller and more streamlined, allowing for better integration with the surrounding bone and gums. This has resulted in improved aesthetics and reduced risk of complications. The development of implants with different shapes and sizes has also expanded treatment options, allowing for better customization to individual patient needs.
- Advanced Aesthetics: The focus on aesthetics has led to the development of implant-supported prostheses that closely resemble natural teeth. Advances in dental ceramics, CAD/CAM technology, and innovative tooth-shaping techniques have made it possible to create highly realistic and aesthetically pleasing restorations.
Digital Technology in Implant-Supported Prostheses
Digital technology has significantly impacted the design and fabrication of implant-supported prostheses.
- Digital Impressions: Intraoral scanners have replaced traditional impression techniques, offering a more accurate and comfortable experience for patients. Digital impressions are captured in 3D, providing precise data for the design and fabrication of restorations.
- Computer-Aided Design (CAD): CAD software allows dentists to create detailed 3D models of implant-supported prostheses, ensuring a precise fit and optimal function. This technology enables customization of the prosthesis to meet individual patient needs.
- Computer-Aided Manufacturing (CAM): CAM technology uses computer-controlled milling machines to fabricate implant-supported prostheses from materials like zirconia or titanium. This process ensures accuracy, consistency, and efficiency in the production of restorations.
Innovative Implant-Supported Prostheses
The field of implant dentistry continues to evolve, with innovative solutions emerging to address diverse patient needs.
- Implant-Retained Overdentures: These prostheses offer a secure and stable solution for patients with complete or partial edentulism. They consist of a denture that is attached to implants using special attachments, such as magnets or clips. This design provides excellent stability and retention, allowing for natural chewing and speech.
- All-on-Four Solutions: This innovative technique involves placing four strategically positioned implants in the jawbone to support a full arch prosthesis. It offers a minimally invasive and efficient solution for patients with complete tooth loss, allowing for immediate function and improved aesthetics.
Types of Implant-Supported Prostheses
| Type | Characteristics | Indications |
|---|---|---|
| Implant-Supported Crown | A single tooth restoration that is attached to a dental implant. | Replacing a single missing tooth. |
| Implant-Supported Bridge | A fixed prosthesis that replaces multiple missing teeth, spanning the gap between two or more implants. | Replacing multiple missing teeth in a row. |
| Implant-Retained Overdenture | A removable prosthesis that is attached to implants using special attachments. | Replacing all teeth in an arch, or multiple teeth in a partially edentulous arch. |
| All-on-Four Prosthesis | A fixed prosthesis that supports a full arch of teeth, using only four strategically placed implants. | Replacing all teeth in an arch, offering a minimally invasive and efficient solution. |
Emerging Technologies in Dental Implants
The field of dental implants is constantly evolving, with exciting new technologies emerging that promise to revolutionize implant dentistry. These advancements are driven by the pursuit of improved outcomes, reduced invasiveness, and enhanced patient experience.
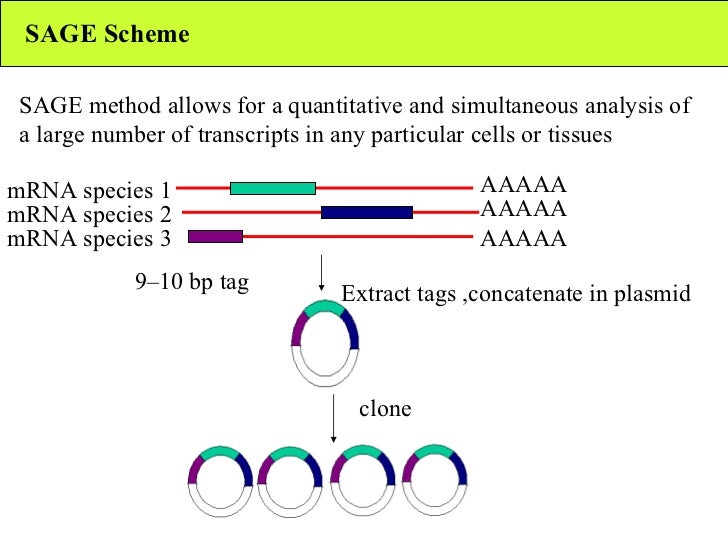
Bioprinting and Tissue Engineering in Implant Dentistry
Bioprinting and tissue engineering are two promising technologies that have the potential to transform implant dentistry. Bioprinting involves the use of 3D printing techniques to create living tissues and organs, while tissue engineering focuses on creating functional tissues from cells and biomaterials.
Bioprinting offers the potential to create customized implants that are perfectly matched to the patient’s anatomy and needs. By printing a scaffold of biocompatible materials, such as collagen or hydroxyapatite, and seeding it with the patient’s own cells, bioprinting can create a living implant that integrates seamlessly with the surrounding bone. This approach could significantly reduce the risk of implant rejection and improve the long-term success rate of implants.
Tissue engineering is another promising approach that could revolutionize implant dentistry. By using stem cells and biomaterials, tissue engineers can create functional tissues that can be used to repair damaged bone or to create new implants. This approach could be particularly beneficial for patients with bone loss or other dental conditions that make traditional implants challenging.
Stem Cell Therapy and Regenerative Medicine in Implant Rehabilitation
Stem cell therapy and regenerative medicine are emerging fields that hold immense potential for implant rehabilitation. Stem cells are undifferentiated cells that have the ability to develop into different cell types, making them ideal for regenerative medicine applications.
Stem cell therapy involves transplanting stem cells into the body to stimulate tissue regeneration. In implant dentistry, stem cells can be used to promote bone regeneration around implants, which can improve implant stability and longevity. Regenerative medicine aims to repair or replace damaged tissues and organs. In implant dentistry, regenerative medicine techniques can be used to regenerate bone, gum tissue, or even teeth.
Future Trends in Implant Dentistry
Several exciting trends are emerging in implant dentistry, driven by advancements in technology and materials science.
- Personalized Implants: Personalized implants are designed to perfectly match the patient’s anatomy and needs. Using 3D imaging and computer-aided design (CAD), dentists can create custom implants that fit precisely into the patient’s jawbone. This approach can improve implant stability, reduce the risk of complications, and shorten the healing time.
- Smart Implants: Smart implants are equipped with sensors and communication technologies that allow them to monitor their own performance and communicate with the patient’s smartphone or other devices. This data can be used to detect potential problems early, allowing for timely intervention and preventing complications.
- Biocompatible Materials: Research is ongoing to develop new biocompatible materials that are more durable, biocompatible, and osseointegrative. These materials will improve implant longevity and reduce the risk of implant rejection.
Ongoing Research and Clinical Trials in Dental Implants
Several research groups and universities are actively engaged in research and clinical trials related to dental implants.
- The University of California, San Francisco (UCSF) is conducting a clinical trial to evaluate the safety and efficacy of bioprinted implants in patients with missing teeth.
- The University of Pennsylvania is investigating the use of stem cell therapy to promote bone regeneration around dental implants.
- The National Institutes of Health (NIH) is funding research on the development of new biocompatible materials for dental implants.
End of Discussion
As we conclude this journey into the world of newest technology in dental implants, one thing is clear: the future of implant dentistry is bright. With continued research and development, we can expect even more innovative solutions that will improve the lives of countless patients. The advancements discussed here are not merely technical feats, but rather transformative tools that are empowering dentists to deliver exceptional care and restore smiles with greater precision and confidence.
The newest technology in dental implants is revolutionizing the way we approach oral health. These advancements are making implants more accessible and affordable, and even more comfortable for patients. Just like the pace technology golf cart has made navigating the golf course a breeze, the latest innovations in dental implants are making a big difference in people’s lives.
With these advancements, we can expect even more innovative solutions to emerge in the future.