New Dental Technology for Missing Teeth: Transforming Smiles
New dental technology for missing teeth has revolutionized the way we address tooth loss, offering innovative solutions that restore both function and aesthetics. From groundbreaking implant materials and minimally invasive […]
New dental technology for missing teeth has revolutionized the way we address tooth loss, offering innovative solutions that restore both function and aesthetics. From groundbreaking implant materials and minimally invasive techniques to the integration of digital dentistry, advancements in this field have significantly improved the patient experience, providing more comfortable, efficient, and predictable outcomes. This exploration delves into the fascinating world of dental implants, showcasing how these cutting-edge technologies are transforming the lives of individuals who have lost teeth.
The evolution of dental implants has been a remarkable journey, starting with early attempts at tooth replacement and culminating in the sophisticated solutions we have today. Traditional implants, made of titanium, have proven highly successful, but newer technologies like mini implants and implant-supported dentures offer additional options for various needs. Digital dentistry has further transformed the field, allowing for greater precision, personalized treatment plans, and enhanced patient comfort. Minimally invasive techniques, such as flapless surgery, have reduced surgical trauma and accelerated healing, leading to improved patient satisfaction. This article explores these advancements, highlighting the latest materials, designs, and procedures that are shaping the future of dental implant technology.
Advanced Implant Materials and Designs: New Dental Technology For Missing Teeth
The evolution of dental implants has been driven by advancements in materials science and engineering. These advancements have led to the development of new implant materials and designs that offer improved biocompatibility, osseointegration, and aesthetic outcomes.
Titanium Alloys
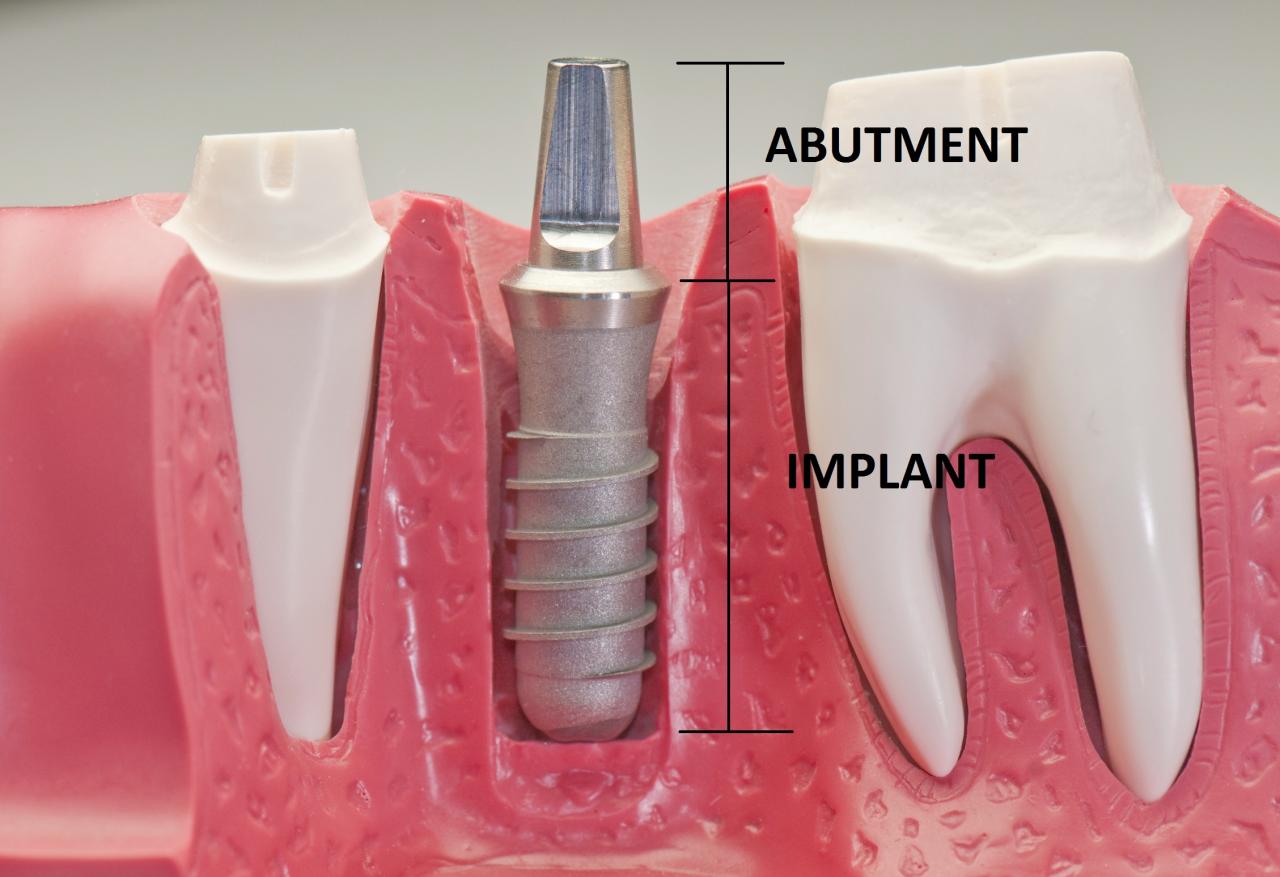
Titanium alloys have long been the gold standard for dental implants due to their excellent biocompatibility and osseointegration properties. These alloys are highly resistant to corrosion and possess a high tensile strength, making them durable and reliable. Titanium’s ability to form a strong bond with bone tissue, known as osseointegration, is crucial for the long-term success of dental implants.
- Titanium alloys are highly biocompatible, meaning they are well-tolerated by the body and do not cause allergic reactions.
- They exhibit excellent osseointegration, forming a strong bond with bone tissue, ensuring implant stability.
- Titanium alloys are strong and durable, able to withstand the forces of chewing and biting.
- They are relatively inexpensive compared to other implant materials.
Zirconia
Zirconia, a ceramic material, has emerged as a viable alternative to titanium alloys in dental implant applications. Zirconia implants offer excellent biocompatibility, high strength, and aesthetic properties. Zirconia’s white color allows for a more natural-looking restoration, particularly in cases where the implant is visible in the smile.
- Zirconia implants are highly biocompatible and do not cause allergic reactions.
- They are very strong and durable, comparable to titanium alloys.
- Zirconia’s white color provides excellent aesthetic properties, matching the natural color of teeth.
- Zirconia is known for its resistance to wear and tear, ensuring long-term implant longevity.
Biocompatible Ceramics
Biocompatible ceramics, such as hydroxyapatite and bioactive glass, are increasingly being used in dental implants. These materials are known for their excellent biocompatibility and ability to promote bone regeneration. Bioceramics are often used as coatings on titanium implants to enhance osseointegration and reduce the risk of implant failure.
- Biocompatible ceramics are highly biocompatible, readily accepted by the body.
- They promote bone regeneration, aiding in the healing process and enhancing osseointegration.
- Bioceramic coatings on titanium implants can improve the surface roughness, enhancing bone contact and osseointegration.
Tapered Implants
Tapered implants, featuring a gradually narrowing design, offer several advantages over traditional cylindrical implants. This design allows for a more stable implant placement, reducing the risk of implant movement and failure. Tapered implants are particularly beneficial in cases where bone density is compromised.
- Tapered implants provide a larger contact area with bone, increasing stability and reducing the risk of implant loosening.
- They offer a more predictable and controlled implant placement, minimizing the risk of complications.
- Tapered implants are well-suited for cases with limited bone volume, allowing for efficient implant placement.
Conical Implants
Conical implants, characterized by their conical shape, are designed to mimic the natural shape of a tooth root. This design allows for a more secure implant placement and enhances the distribution of forces, reducing the risk of implant failure.
- Conical implants provide a more secure and stable implant placement, minimizing the risk of implant loosening.
- They distribute forces more evenly, reducing the stress on the implant and surrounding bone tissue.
- Conical implants are particularly beneficial in cases with compromised bone density, providing increased stability.
Implants with Surface Modifications
Surface modifications, such as micro-roughening and coatings, have been developed to enhance osseointegration and improve the long-term success of dental implants. These modifications increase the surface area of the implant, promoting bone cell attachment and accelerating bone healing.
- Micro-roughened surfaces provide a greater surface area for bone cells to attach, enhancing osseointegration.
- Coatings, such as hydroxyapatite, can promote bone regeneration and accelerate the healing process.
- Surface modifications contribute to a more stable implant placement, reducing the risk of implant failure.
Bone Grafting and Regeneration
Bone grafting is a crucial procedure in implant dentistry, particularly when dealing with bone loss. Bone loss can occur due to various factors, including periodontal disease, tooth extraction, trauma, or congenital defects. When the jawbone lacks sufficient density and volume to support an implant, bone grafting is necessary to create a stable foundation for implant placement.
Types of Bone Grafting Materials
Bone grafting materials are used to augment the jawbone and provide a suitable environment for new bone growth. Different materials are used, each with its own advantages and disadvantages.
- Autografts: These are bone grafts harvested from the patient’s own body, typically from the iliac crest (hip bone), chin, or jaw. Autografts are considered the “gold standard” because they have the highest osteoconductive and osteoinductive properties, meaning they are excellent at promoting bone growth. However, they involve a second surgical site, which can lead to pain, discomfort, and potential complications.
- Allografts: These are bone grafts harvested from a deceased human donor. Allografts are treated to eliminate the risk of disease transmission and are readily available. They are less osteoinductive than autografts but still offer good osteoconductive properties.
- Xenografts: These are bone grafts derived from animal sources, usually bovine (cow) or porcine (pig). Xenografts are treated to reduce the risk of immune rejection and are readily available. They are less osteoinductive than autografts and allografts but offer good osteoconductive properties.
- Synthetic Bone Substitutes: These are materials created in a laboratory, such as calcium phosphate ceramics, hydroxyapatite, and bioactive glass. They are biocompatible and readily available. However, they are generally less osteoinductive than natural bone grafts.
Bone Grafting Techniques
The choice of bone grafting technique depends on the extent of bone loss, the location of the implant, and the patient’s overall health.
- Block Grafting: This technique involves using a large block of bone to fill the defect. It is often used for larger bone defects and can provide excellent support for implants.
- Particulate Grafting: This technique involves using small bone particles to fill the defect. It is often used for smaller defects and can be combined with other techniques.
- Guided Bone Regeneration (GBR): This technique involves using a membrane to create a space for bone to grow. The membrane acts as a barrier, preventing soft tissue from growing into the space and allowing bone to regenerate. GBR is often used in conjunction with bone grafting materials.
Growth Factors and Stem Cells in Bone Regeneration
Growth factors and stem cells play a crucial role in enhancing bone regeneration and promoting implant stability.
- Growth Factors: These are proteins that stimulate bone cell growth and differentiation. They can be derived from various sources, including bone marrow, platelets, and synthetically produced. Growth factors can be used in conjunction with bone grafting materials to accelerate bone healing.
- Stem Cells: These are undifferentiated cells that can differentiate into various cell types, including bone cells. Stem cells can be harvested from bone marrow, adipose tissue, or dental pulp. They can be used to promote bone regeneration by providing a source of new bone-forming cells.
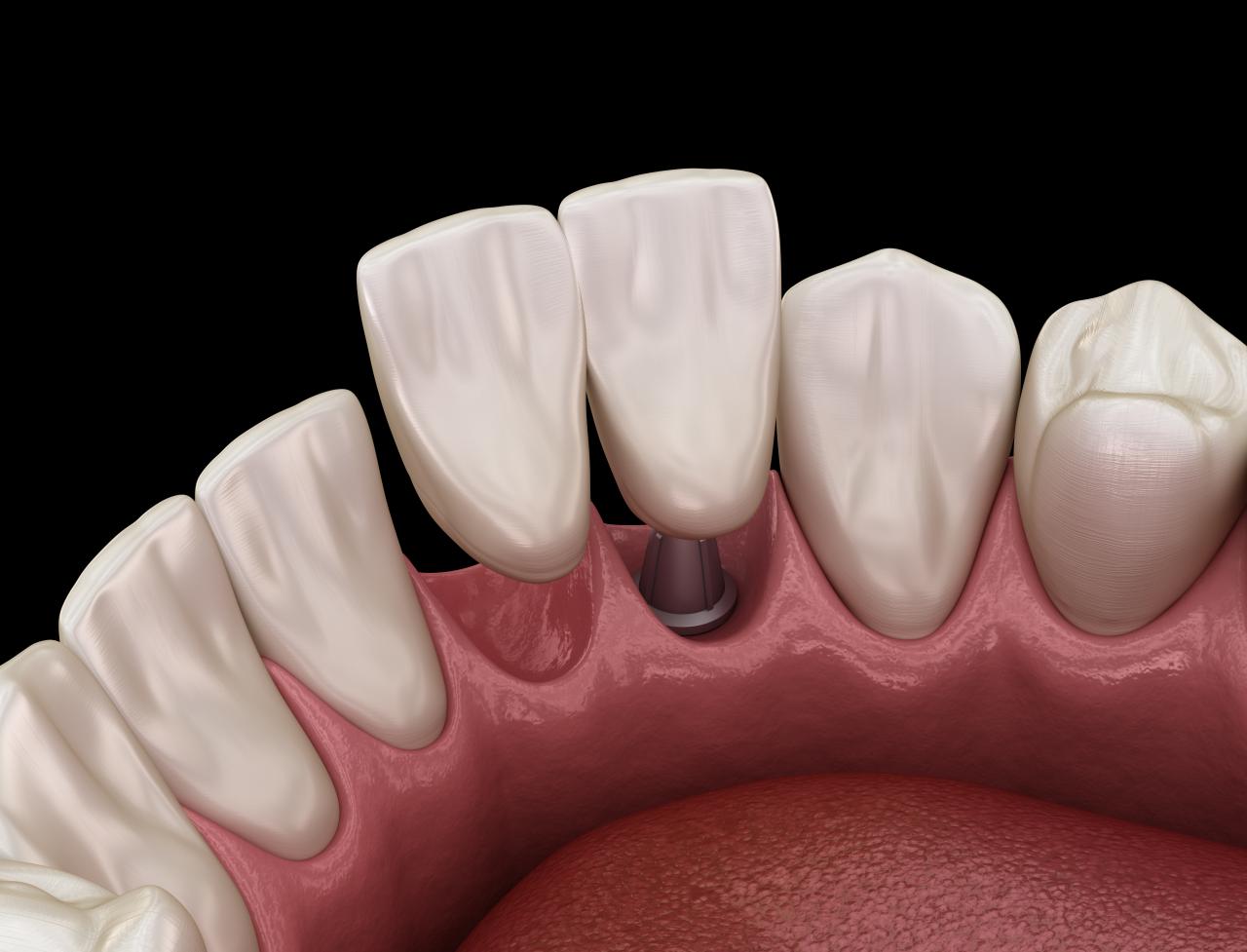
Implant-Supported Restorations

Once the dental implant has successfully integrated with the jawbone, it’s time to consider the final restoration, the visible part that replaces the missing tooth or teeth. There are various types of implant-supported restorations, each offering distinct advantages and disadvantages based on factors like aesthetics, functionality, and cost.
Types of Implant-Supported Restorations
The type of implant-supported restoration best suited for a patient depends on several factors, including the number of missing teeth, the location of the missing teeth, the patient’s overall oral health, and their budget. Here are the most common types of implant-supported restorations:
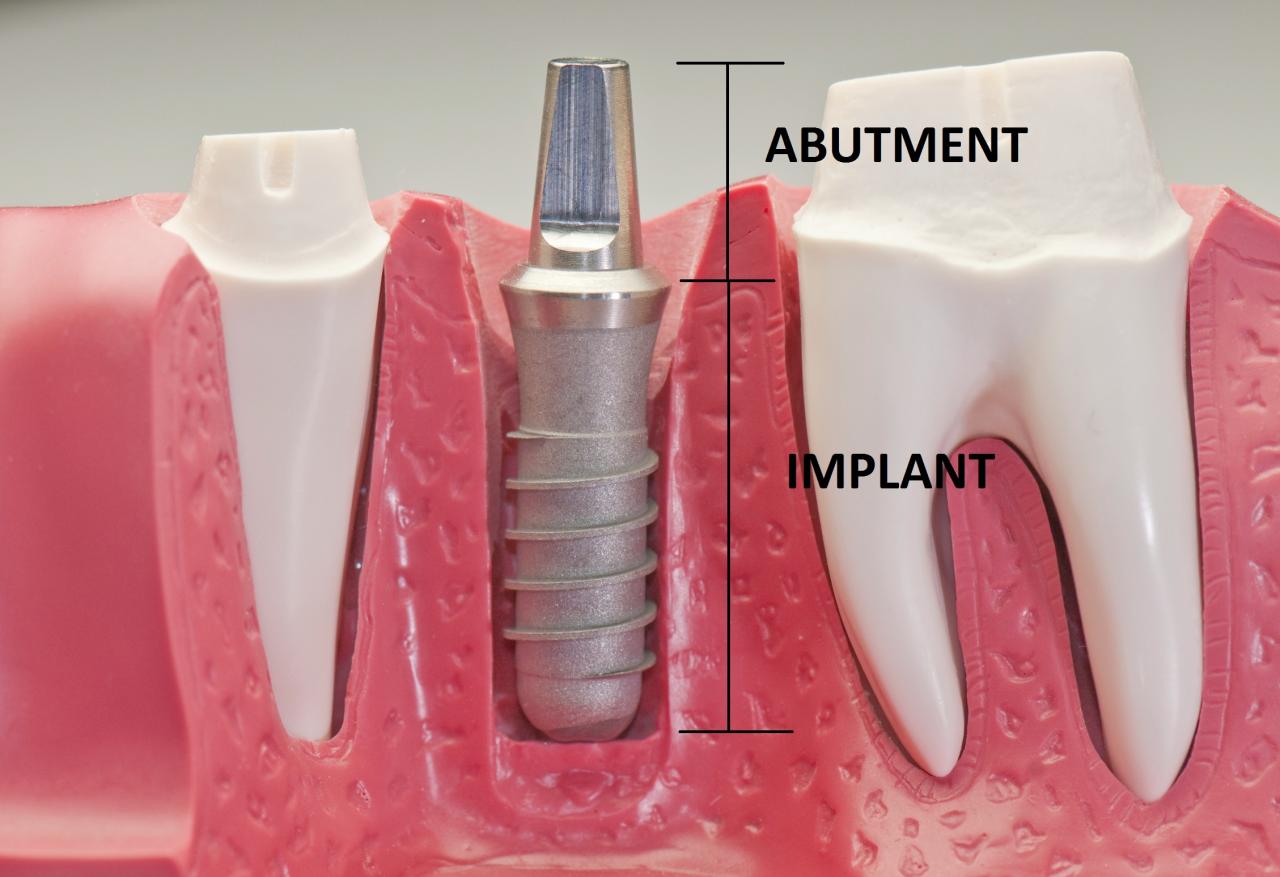
- Crowns: These are single-tooth restorations that are used to replace a single missing tooth. Crowns are typically made of porcelain or ceramic, which are strong and aesthetically pleasing. They are cemented onto an abutment, which is a small connector that attaches the crown to the implant.
- Bridges: Bridges are used to replace multiple missing teeth in a row. They consist of two or more crowns that are joined together by a pontic, which is an artificial tooth that fills the gap. Bridges can be supported by one or more dental implants.
- Dentures: Dentures are removable appliances that are used to replace a full arch of missing teeth. Implant-supported dentures are secured to dental implants, which provides a more stable and secure fit than traditional dentures. Implant-supported dentures can be either fixed (permanently attached) or removable.
Advantages and Disadvantages of Implant-Supported Restorations
Each type of implant-supported restoration has its own set of advantages and disadvantages:
Crowns
- Advantages:
- Highly aesthetic
- Durable and long-lasting
- Natural-looking and feel
- Preserve surrounding teeth
- Disadvantages:
- More expensive than other options
- Requires multiple procedures
- Not suitable for all patients
Bridges
- Advantages:
- Natural-looking and functional
- More affordable than multiple crowns
- Preserve surrounding teeth
- Disadvantages:
- May require more extensive tooth preparation
- Can be difficult to clean
- Not as durable as crowns
Dentures
- Advantages:
- Affordable option
- Can replace multiple missing teeth
- Removable for cleaning and maintenance
- Disadvantages:
- Not as secure as other options
- May require adjustments over time
- Can affect speech and chewing
Role of Dental Labs and Technicians, New dental technology for missing teeth
Dental labs and technicians play a crucial role in the fabrication of high-quality implant restorations. They use advanced technology and materials to create custom restorations that perfectly fit the patient’s mouth. Dental technicians work closely with dentists to ensure that the restorations meet the patient’s individual needs and expectations.
Future Trends in Dental Implant Technology

The field of dental implants is constantly evolving, with new technologies emerging that promise to revolutionize the way we treat missing teeth. From biomimicry to artificial intelligence, these advancements hold the potential to significantly improve implant procedures, treatment outcomes, and the overall patient experience.
Biomimicry in Dental Implants
Biomimicry, the practice of learning from nature to solve human problems, is gaining traction in the dental implant field. By mimicking the structure and function of natural teeth, researchers aim to develop implants that are more biocompatible, durable, and aesthetically pleasing.
- One example is the development of implants with surfaces that mimic the enamel of natural teeth. These surfaces are designed to promote the growth of healthy bone tissue, leading to stronger and more stable implants.
- Another area of focus is the creation of implants with a more natural appearance. Researchers are developing implants with customized shapes and colors that blend seamlessly with the surrounding teeth.
Artificial Intelligence in Dental Implant Planning and Surgery
Artificial intelligence (AI) is transforming various aspects of healthcare, and dentistry is no exception. AI algorithms are being used to analyze patient data, such as CT scans and medical history, to create personalized treatment plans and predict potential complications.
- AI-powered software can assist surgeons in planning implant placement with greater precision, minimizing the risk of damage to surrounding tissues and nerves.
- AI-driven robotic systems are being developed to perform certain aspects of implant surgery, such as drilling and bone preparation, with increased accuracy and control.
Personalized Medicine in Dental Implant Treatment
Personalized medicine, which tailors treatment to an individual’s unique genetic makeup and lifestyle, is also impacting the field of dental implants. This approach allows for more targeted and effective treatment, improving outcomes and minimizing side effects.
- Genetic testing can identify patients at risk for implant failure, enabling preventative measures and personalized treatment strategies.
- Researchers are exploring the use of stem cell therapy to promote bone regeneration around implants, leading to faster healing and improved implant stability.
Ethical Considerations and Challenges
While these advancements hold immense promise, they also raise ethical considerations and challenges.
- One concern is the potential for bias in AI algorithms, which could lead to disparities in treatment outcomes for different patient groups.
- Another challenge is ensuring the safety and efficacy of new technologies before they are widely adopted. Rigorous clinical trials are essential to validate the effectiveness and safety of these emerging technologies.
Final Review
The future of dental implant technology is bright, with ongoing research and development promising even more advanced solutions. From biomimicry and artificial intelligence to personalized medicine, the field is poised to further enhance the patient experience, offering greater comfort, faster recovery, and more predictable outcomes. As we continue to explore the potential of these innovations, we can look forward to a future where tooth loss is no longer a barrier to a healthy, confident smile. The impact of these technologies extends beyond aesthetics, improving overall oral health and quality of life for individuals who have lost teeth. The journey of dental implants has come a long way, and the future holds even greater promise for restoring smiles and enhancing lives.
New dental technology for missing teeth has revolutionized the way we approach oral health. From implants to dentures, the options are vast, and the quality of these solutions has drastically improved. For those interested in learning more about the business side of this industry, the American Business & Technology University offers programs in healthcare administration, which can be a great stepping stone to a career in this growing field.
With the increasing demand for these technologies, there’s a lot of opportunity for professionals who can understand both the science and the business behind these advancements.