New Dental Implant Technology 2024: Revolutionizing Oral Health
New dental implant technology 2024 is ushering in a new era of oral health, offering patients innovative solutions for missing teeth with enhanced comfort, durability, and aesthetics. The advancements in […]

New dental implant technology 2024 is ushering in a new era of oral health, offering patients innovative solutions for missing teeth with enhanced comfort, durability, and aesthetics. The advancements in implant materials, minimally invasive techniques, and digital dentistry are transforming the implant experience, making it more accessible and predictable than ever before.
From biocompatible materials like zirconia to personalized implant designs, the field is rapidly evolving, catering to individual needs and improving implant success rates. This article explores the latest developments in dental implant technology, highlighting the key innovations and their impact on patient care.
Advancements in Implant Materials
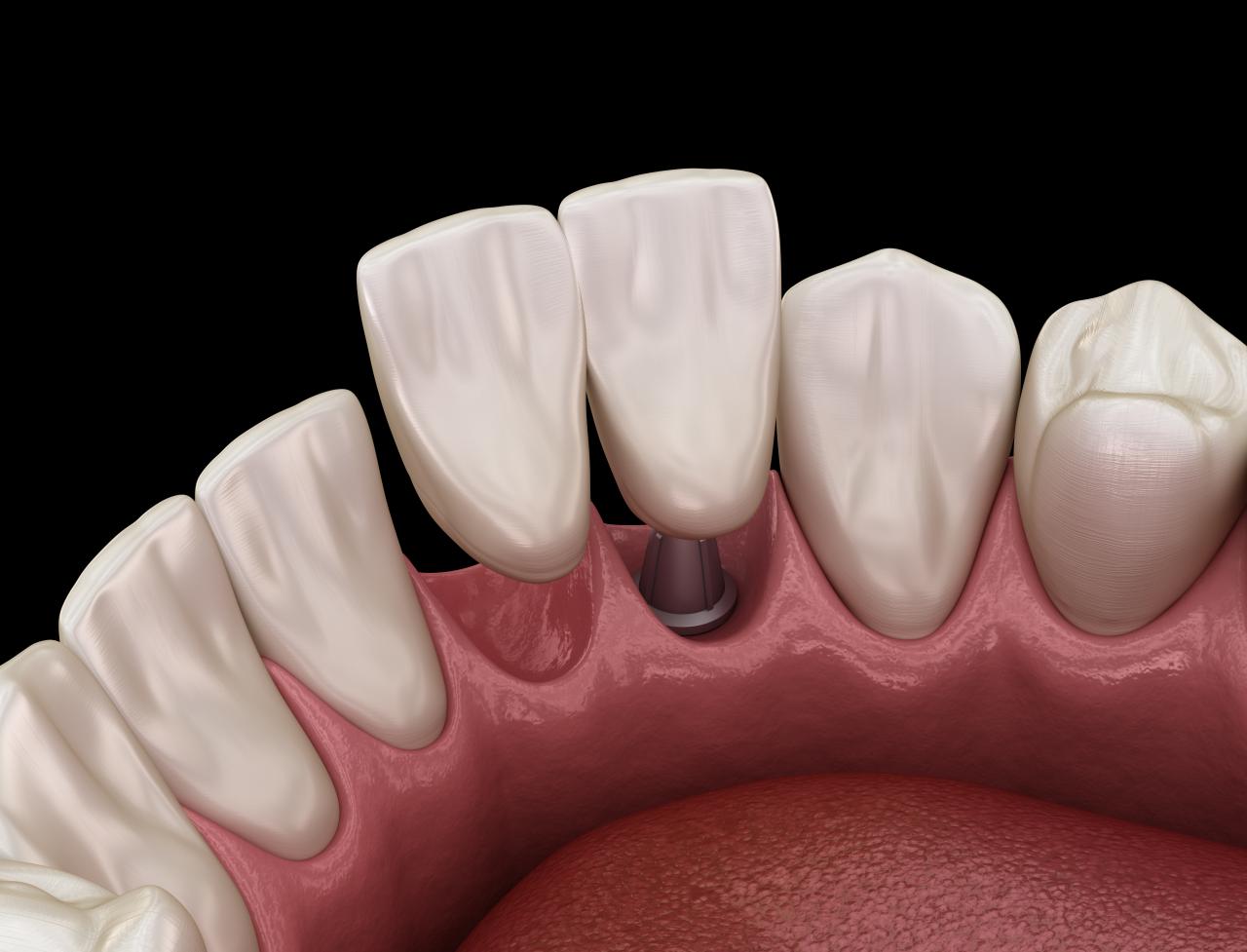
Dental implants have revolutionized tooth replacement, offering a durable and aesthetically pleasing solution. As technology advances, so do the materials used in implant construction. This evolution aims to enhance biocompatibility, longevity, and overall patient comfort.
Titanium Implants
Titanium remains the gold standard for dental implants due to its exceptional biocompatibility and osseointegration properties. Titanium implants readily integrate with the surrounding bone, forming a strong and stable foundation for the artificial tooth. However, titanium can have certain limitations. For example, it can cause allergic reactions in a small percentage of patients. Additionally, titanium’s metallic appearance may be aesthetically unappealing, particularly in areas where the gum tissue is thin.
Zirconia Implants
Zirconia, a ceramic material, has emerged as a viable alternative to titanium implants. Zirconia implants are highly biocompatible, hypoallergenic, and aesthetically pleasing, as they have a natural tooth-like appearance. They are also known for their exceptional strength and durability, making them a suitable option for patients with limited bone density. However, zirconia implants can be more expensive than titanium implants, and their osseointegration rate may be slightly lower.
Other Emerging Materials
Researchers are exploring other promising materials for dental implants, including:
- Bioactive Glass: Bioactive glass is a material that promotes bone growth and integration, potentially leading to faster healing and improved osseointegration.
- Polyethylene Glycol (PEG): PEG is a biocompatible polymer that can be used to create coatings for dental implants, reducing the risk of bacterial infection and improving osseointegration.
- Nanomaterials: Nanomaterials, such as carbon nanotubes and graphene, offer enhanced mechanical properties and biocompatibility, making them promising candidates for future implant development.
These advancements in implant materials are driving the development of more personalized and effective dental implant solutions. As research progresses, we can expect even more innovative and biocompatible materials to emerge, further enhancing the long-term success and patient satisfaction associated with dental implants.
Minimally Invasive Implant Placement Techniques
The evolution of dental implant technology has brought about a paradigm shift in implant placement techniques, prioritizing minimally invasive approaches for enhanced patient comfort and faster recovery. These advancements are driven by a focus on minimizing surgical trauma, reducing pain, and optimizing healing outcomes.
Guided Surgery
Guided surgery leverages digital technology to plan and execute implant placement procedures with precision. The process involves creating a 3D model of the patient’s jawbone using advanced imaging techniques like cone-beam computed tomography (CBCT). This virtual model allows the dentist to plan the implant placement precisely, ensuring optimal positioning and minimizing the risk of complications.
A surgical guide is then created based on the 3D model, which acts as a template during the procedure, guiding the dentist to the pre-determined implant sites. This ensures accurate implant placement and minimizes the need for extensive bone removal or tissue manipulation.
Guided surgery is particularly beneficial for complex implant cases, such as those involving limited bone volume or challenging anatomical features.
Computer-Aided Design/Computer-Aided Manufacturing (CAD/CAM)
CAD/CAM technology plays a crucial role in minimally invasive implant placement, enabling the fabrication of custom-made surgical guides and implant components. The process involves using digital imaging to capture precise measurements of the patient’s jawbone, which are then used to design and manufacture customized components.
This personalized approach ensures a perfect fit for each patient, minimizing the need for adjustments during surgery. CAD/CAM also allows for the creation of implants with specific shapes and sizes, optimizing integration with the surrounding bone.
Robotic Assistance
Robotic assistance in implant placement represents a cutting-edge advancement in minimally invasive dentistry. These robotic systems offer enhanced precision and control during the procedure, allowing for more accurate implant placement.
The robots are programmed with the surgical plan, ensuring that the implants are placed in the predetermined locations. This technology is particularly advantageous for complex implant cases, where precision and accuracy are paramount.
Robotic-assisted implant placement is still a relatively new technology, but it holds immense potential for improving patient outcomes and streamlining the implant procedure.
Digital Dentistry and Implant Planning
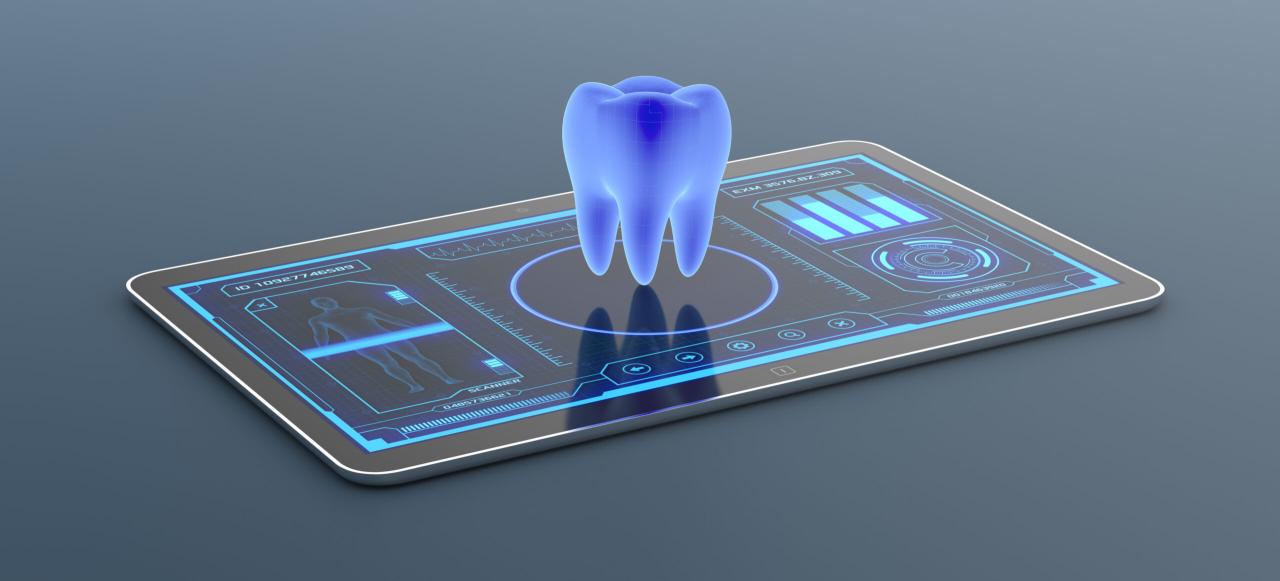
The realm of dental implant treatment has been revolutionized by the integration of digital technologies, enabling more precise planning, efficient placement, and improved patient communication. This section delves into the key role of digital imaging, 3D scans, and specialized software in shaping the modern implant journey.
Digital Imaging and 3D Scans
Digital imaging, specifically 3D scans, provides a comprehensive and detailed representation of the patient’s oral anatomy. This technology captures intricate details of bone structure, tooth position, and soft tissue contours, creating a virtual model of the patient’s mouth. This virtual model serves as the foundation for meticulous implant planning, allowing dentists to:
- Assess bone density and volume to determine the ideal implant placement locations.
- Identify potential obstacles or anatomical limitations that may influence implant placement.
- Virtually simulate the final implant position, ensuring optimal aesthetics and functionality.
Software-Driven Implant Planning
Specialized software applications leverage the power of digital imaging and 3D scans to facilitate precise implant planning. These software programs enable dentists to:
- Design a virtual implant surgical guide, a customized template that guides the placement of implants with pinpoint accuracy.
- Predict the potential outcomes of implant placement, including the final crown position and overall smile aesthetics.
- Communicate complex treatment plans to patients in a clear and easily understandable manner, fostering informed decision-making.
Benefits of Digital Dentistry in Implant Treatment
| Benefit | Description |
|---|---|
| Enhanced Accuracy | Digital planning and guided surgery significantly minimize the margin of error, leading to more precise implant placement. |
| Reduced Surgical Time | Pre-operative planning and virtual surgical guides streamline the surgical procedure, resulting in shorter surgery durations and quicker recovery times. |
| Improved Patient Communication | 3D models and virtual simulations allow patients to visualize the entire treatment process, promoting understanding and confidence in the planned procedure. |
| Minimized Complications | Precise implant placement reduces the risk of complications, such as nerve damage or implant failure, leading to a smoother and more predictable recovery. |
| Enhanced Aesthetics | Virtual planning ensures that implants are placed in the optimal position for a natural and aesthetically pleasing smile. |
Improved Implant Integration and Osseointegration
Dental implant success hinges on the establishment of a strong and lasting bond between the implant and the surrounding bone. This process, known as osseointegration, is crucial for long-term implant stability and functionality. Recent advancements in implant technology have focused on enhancing osseointegration, aiming for faster healing times, improved implant stability, and reduced risks of implant failure.
Surface Modifications and Coatings
Surface modifications and coatings play a significant role in promoting osseointegration. These techniques aim to enhance the implant surface’s biocompatibility and osteoconductivity, fostering a more favorable environment for bone cells to adhere, proliferate, and integrate with the implant.
- Micro-roughening: Creating microscopic irregularities on the implant surface increases its surface area, providing more sites for bone cells to attach. This enhanced surface topography promotes cell adhesion and bone growth.
- Nano-structured coatings: Applying nano-scale coatings, such as hydroxyapatite (HA) or titanium dioxide (TiO2), can further enhance the implant’s bioactivity and osteoconductivity. These coatings mimic the natural composition of bone, encouraging bone cell attachment and growth.
- Bioactive coatings: Incorporating bioactive molecules, like growth factors or proteins, into the implant surface can stimulate bone regeneration and accelerate osseointegration. These coatings promote cell signaling pathways that encourage bone formation and healing.
Osseointegration and Its Significance
Osseointegration is a biological process where a direct structural and functional connection forms between the implant material and living bone. This process is essential for dental implant success as it ensures the implant remains securely anchored in the jawbone, providing stability and support for prosthetic teeth.
“Osseointegration is the process of direct bone bonding to an implant material, without intervening soft tissue.” – Brånemark, P. I. (1982)
- Stability and Function: Osseointegration provides the necessary stability for implants to withstand chewing forces and prevent implant loosening or failure. This stability allows for the placement of prosthetic teeth that function naturally and comfortably.
- Durability and Longevity: A successful osseointegration process leads to a long-lasting implant, reducing the risk of complications and ensuring the implant’s functionality over time.
- Improved Aesthetics: Stable implants support prosthetic teeth, providing a natural appearance and improving the overall aesthetics of the smile.
Factors Influencing Osseointegration
Several factors can influence the success of osseointegration, including:
- Implant Material: Titanium is the most commonly used material for dental implants due to its biocompatibility and excellent osseointegration properties. However, newer materials like zirconia are also gaining popularity for their aesthetic qualities and potential for improved osseointegration.
- Implant Design: The implant’s shape, size, and surface topography can influence bone growth and osseointegration. Advanced implant designs are optimized for optimal bone contact and faster healing.
- Surgical Technique: Proper surgical technique is crucial for successful osseointegration. Precise implant placement, minimal trauma to the surrounding bone, and adequate blood supply are essential for optimal healing.
- Patient Health: Underlying medical conditions, such as diabetes or smoking, can affect bone healing and osseointegration. Proper patient management and addressing these factors are crucial for successful implant outcomes.
Personalized Implant Solutions

The field of dental implants is witnessing a paradigm shift with the emergence of personalized implant solutions, which are designed to cater to the unique needs of each patient. This personalized approach goes beyond standard implant sizes and shapes, offering customized implants that address specific anatomical variations and bone densities.
Tailored Implants for Individual Needs
Personalized implant solutions leverage advanced technologies to create implants that are specifically tailored to a patient’s unique anatomy and bone density. These implants are designed to provide a more precise fit, enhancing stability, reducing the risk of complications, and improving long-term outcomes.
- Customized Implant Design: Advanced imaging techniques, such as cone-beam computed tomography (CBCT), are used to create 3D models of a patient’s jawbone. These models allow for the design of implants with specific dimensions, shapes, and angles that perfectly match the patient’s anatomy. This ensures optimal implant placement and bone integration.
- Bone Density-Specific Implants: Patients with different bone densities require different implant designs. For patients with low bone density, implants with a larger diameter or a specialized surface coating can be designed to promote better bone integration and reduce the risk of implant failure. Conversely, patients with high bone density may require implants with a smaller diameter for optimal fit.
- Anatomically Customized Implants: The jawbone’s anatomy varies significantly from person to person. Personalized implant solutions can address these variations by designing implants that accommodate specific anatomical features, such as the presence of nerves, blood vessels, or sinuses. This minimizes the risk of damage to surrounding tissues and improves the overall success rate of the implant procedure.
Benefits of Personalized Implant Treatments, New dental implant technology 2024
Personalized implant solutions offer a range of benefits for patients, including:
- Improved Implant Stability: Customized implants provide a more precise fit, resulting in greater stability and reduced risk of implant movement or loosening. This leads to a more comfortable and predictable outcome.
- Enhanced Bone Integration: The tailored design of personalized implants promotes optimal bone integration, which is essential for long-term implant success. This reduces the risk of implant failure and ensures the implant remains securely in place for many years.
- Reduced Risk of Complications: Personalized implants minimize the risk of complications such as nerve damage, sinus perforation, or implant rejection. This is because they are designed to perfectly match the patient’s anatomy and avoid potential conflict with surrounding tissues.
- Improved Aesthetic Outcomes: Personalized implants can be designed to enhance the aesthetics of the smile by matching the natural shape and contour of the teeth. This is particularly important for patients who have lost multiple teeth and are seeking a natural-looking restoration.
Challenges of Personalized Implant Treatments
While personalized implant solutions offer significant advantages, they also present certain challenges:
- Increased Cost: The customized design and fabrication process of personalized implants can be more expensive than traditional implants. This is due to the advanced technologies and materials used in their creation.
- Longer Treatment Time: The process of planning and designing personalized implants requires additional time compared to traditional implants. This may involve multiple appointments for imaging, planning, and fabrication.
- Limited Availability: Personalized implant solutions are not yet widely available in all dental practices. This is due to the specialized equipment and expertise required to design and place these implants.
Innovative Implant Restorations: New Dental Implant Technology 2024
The realm of dental implant restorations has undergone a remarkable transformation, driven by advancements in materials, technology, and aesthetic considerations. These innovations aim to deliver not only functional solutions but also aesthetically pleasing results that seamlessly integrate with the patient’s natural dentition.
Advanced Materials for Enhanced Aesthetics and Durability
The choice of materials for implant restorations plays a crucial role in determining their aesthetic appeal, durability, and biocompatibility.
- Zirconia: Known for its exceptional strength, biocompatibility, and natural tooth-like appearance, zirconia has emerged as a popular choice for implant crowns and bridges. Its high translucency allows for the creation of restorations that mimic the natural light-reflecting properties of teeth, resulting in a more lifelike appearance.
- Ceramics: Ceramic materials, such as lithium disilicate, offer excellent aesthetics and biocompatibility. They are highly resistant to staining and can be fabricated into restorations that closely match the color and translucency of natural teeth.
- Composite Resin: Composite resins, often used in traditional dental restorations, are also employed in implant restorations, particularly for smaller restorations or those requiring a more conservative approach. They offer versatility in terms of color matching and can be easily repaired if necessary.
Digital Dentistry and Custom Implant Restorations
Digital dentistry has revolutionized the design and fabrication of implant restorations, enabling greater precision, customization, and efficiency.
- Digital Impressions: Digital impressions using intraoral scanners have replaced traditional impression techniques, providing highly accurate and detailed digital models of the patient’s mouth. This eliminates the need for messy impression materials and allows for immediate visualization of the implant site and surrounding teeth.
- CAD/CAM Technology: Computer-aided design (CAD) and computer-aided manufacturing (CAM) technology enables the creation of highly customized implant restorations based on the digital models. This allows for precise fit, optimal aesthetics, and improved functionality.
- Guided Implant Surgery: Digital planning and guided surgery techniques utilize 3D imaging and software to create surgical guides that aid in the precise placement of implants. This minimizes surgical invasiveness, reduces the risk of complications, and ensures optimal implant positioning for future restoration.
Emerging Technologies in Implant Care
The field of dental implant care is constantly evolving, with new technologies emerging to enhance implant maintenance, hygiene, and longevity. These advancements aim to improve patient compliance and overall implant success rates, ensuring long-lasting smiles and improved oral health.
Laser Cleaning
Laser cleaning offers a non-invasive and highly effective method for removing plaque and bacteria from dental implants. The focused laser beam precisely targets and removes the biofilm without damaging the surrounding tissues. This technology is particularly beneficial for patients with limited dexterity or those who find traditional brushing techniques challenging.
Antibacterial Coatings
Antibacterial coatings applied to dental implants provide an additional layer of protection against bacterial growth. These coatings often utilize materials like silver nanoparticles or antimicrobial peptides, which release antimicrobial agents to inhibit bacterial colonization. This technology can significantly reduce the risk of peri-implantitis, a serious infection that can lead to implant failure.
Benefits and Drawbacks of Emerging Implant Care Technologies
The table below highlights the benefits and drawbacks of various emerging implant care technologies:
| Technology | Benefits | Drawbacks |
|---|---|---|
| Laser Cleaning |
|
|
| Antibacterial Coatings |
|
|
Future Trends in Dental Implant Technology
The field of dental implant technology is constantly evolving, driven by advancements in materials science, digital technologies, and a growing understanding of biological processes. This ongoing evolution is paving the way for even more effective, minimally invasive, and personalized implant solutions in the future.
Artificial Intelligence in Implant Dentistry
Artificial intelligence (AI) is poised to revolutionize various aspects of implant dentistry, from planning to treatment. AI-powered tools can analyze patient data, including medical history, scans, and images, to predict implant success rates, identify potential complications, and recommend optimal treatment plans.
- AI-driven software can analyze 3D scans and create personalized implant plans, ensuring accurate placement and minimizing surgical intervention.
- AI algorithms can analyze patient data to predict implant longevity and personalize maintenance schedules, leading to better long-term outcomes.
Nanotechnology in Implant Materials
Nanotechnology is revolutionizing the development of implant materials, enabling the creation of implants with enhanced properties. Nanomaterials can improve implant biocompatibility, promote osseointegration, and enhance the longevity of implants.
- Nanoparticles can be incorporated into implant surfaces to create a more biocompatible environment, encouraging bone growth and reducing inflammation.
- Nanotechnology can create coatings that resist bacterial adhesion, reducing the risk of implant infections.
Bioprinting for Personalized Implants
Bioprinting is a revolutionary technology that uses 3D printing techniques to create living tissues and organs. In implant dentistry, bioprinting has the potential to create personalized implants tailored to each patient’s anatomy and needs.
- Bioprinting can create customized implants that perfectly match the patient’s bone structure, improving fit and stability.
- Bioprinting can be used to create implants with integrated blood vessels, promoting faster healing and improved osseointegration.
Ultimate Conclusion
The future of dental implant technology is brimming with exciting possibilities. As research continues to push boundaries, we can anticipate even more personalized, minimally invasive, and technologically advanced solutions. With ongoing advancements in materials, techniques, and digital integration, the future of dental implants promises a brighter smile and a healthier life for all.
New dental implant technology in 2024 is rapidly evolving, with advancements in materials and techniques offering more precise and comfortable procedures. Companies like emhart technologies are contributing to this progress by providing cutting-edge equipment and solutions that enable dental professionals to deliver the best possible outcomes for their patients.
This focus on innovation is driving the development of even more sophisticated dental implants, ensuring a brighter future for oral health.