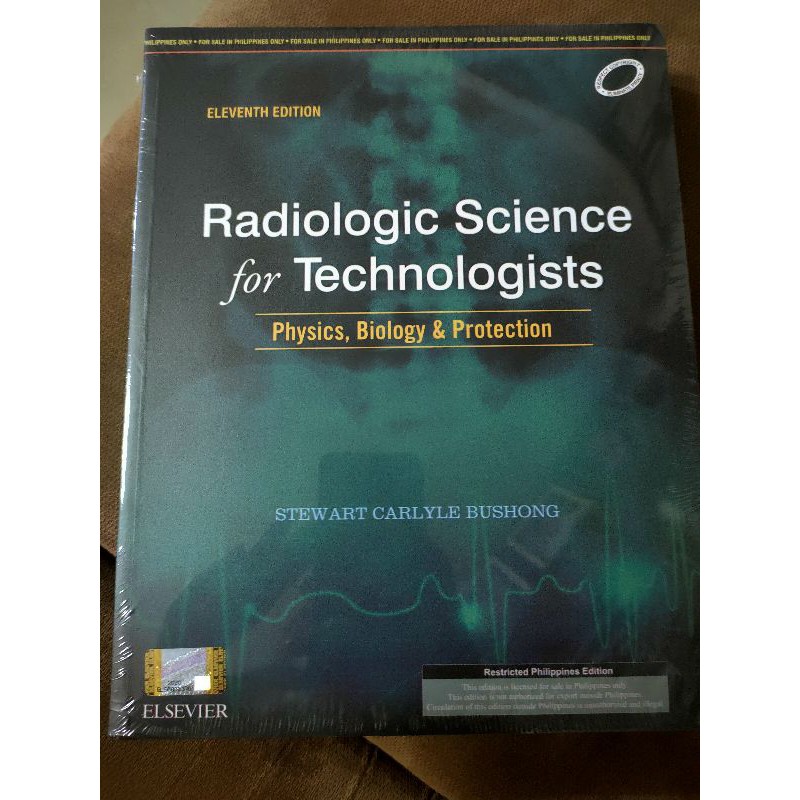
Introduction to Radiologic Technology 8th Edition: A Comprehensive Guide
Introduction to Radiologic Technology 8th Edition takes you on a journey through the fascinating world of medical imaging. This comprehensive guide delves into the history, principles, and practices of radiologic […]
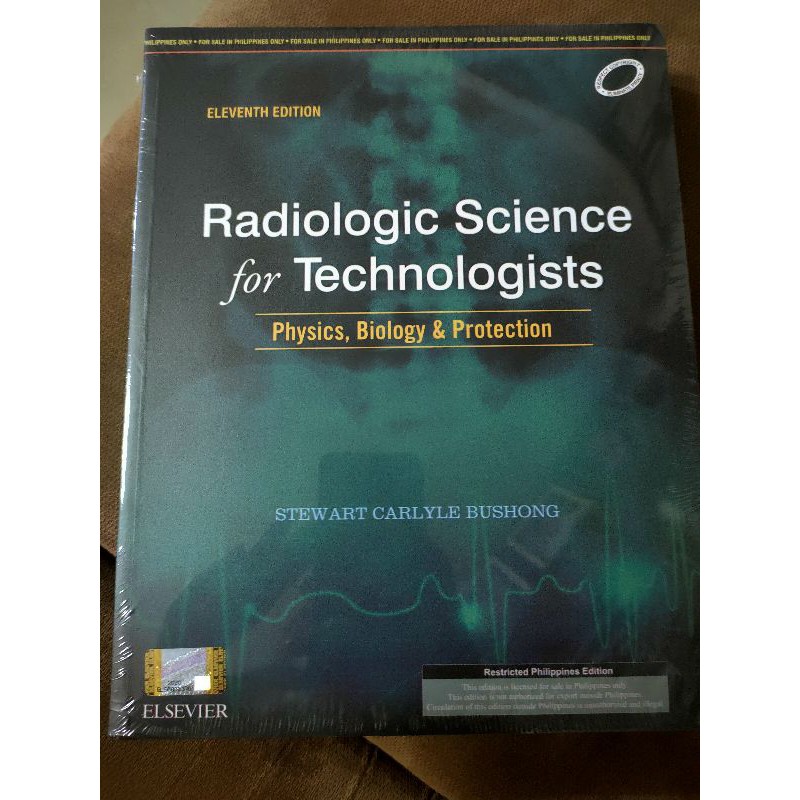
Introduction to Radiologic Technology 8th Edition takes you on a journey through the fascinating world of medical imaging. This comprehensive guide delves into the history, principles, and practices of radiologic technology, equipping you with the knowledge and skills needed to excel in this dynamic field. From understanding the fundamentals of radiation physics to mastering advanced imaging techniques, this book provides a solid foundation for a successful career in radiologic technology.
The book covers a wide range of topics, including the role of radiologic technologists in healthcare, ethical considerations in radiologic practice, image formation and quality, radiographic positioning and technique, radiation safety and protection, quality assurance, and professional development. Through clear explanations, detailed illustrations, and real-world examples, the authors make complex concepts accessible and engaging.
Image Formation and Quality
Understanding image formation and the factors that influence image quality is crucial for radiologic technologists. It allows for the production of high-quality images that are essential for accurate diagnosis and treatment planning. This section explores the fundamental principles of image formation in various radiologic modalities and delves into the key aspects that determine image quality.
Image Formation in Different Radiologic Modalities
Image formation in radiologic modalities relies on the interaction of radiation with matter. The type of radiation used and the interaction process vary depending on the modality.
- Radiography: In conventional radiography, X-rays are emitted from a source and pass through the patient’s body. The amount of radiation that reaches the image receptor (film or digital detector) depends on the tissue density. Dense tissues, such as bone, absorb more radiation, resulting in a lighter area on the image. Less dense tissues, such as soft tissues, absorb less radiation, resulting in a darker area on the image.
- Fluoroscopy: Fluoroscopy uses a continuous beam of X-rays to produce real-time images. This allows for visualization of moving structures, such as the heart and digestive system. Fluoroscopy is often used during surgical procedures and interventional radiology procedures.
- Computed Tomography (CT): CT uses a rotating X-ray source and detectors to acquire multiple images from different angles. These images are then processed by a computer to create cross-sectional images of the body. CT provides detailed anatomical information and is used for diagnosing a wide range of conditions, including cancer, trauma, and cardiovascular disease.
- Magnetic Resonance Imaging (MRI): MRI uses a strong magnetic field and radio waves to create images of the body. The hydrogen atoms in water molecules align themselves with the magnetic field. When radio waves are applied, these atoms release energy, which is detected by the MRI scanner. MRI provides excellent contrast between soft tissues and is used for diagnosing a wide range of conditions, including brain tumors, multiple sclerosis, and spinal cord injuries.
- Ultrasound: Ultrasound uses high-frequency sound waves to create images of the body. Sound waves are reflected back from different tissues, and the time it takes for the waves to return is used to create an image. Ultrasound is used for a variety of purposes, including imaging the fetus during pregnancy, examining the heart, and diagnosing abdominal problems.
- Nuclear Medicine: Nuclear medicine uses radioactive tracers to create images of the body. The tracers are injected into the bloodstream and accumulate in specific organs or tissues. The radiation emitted by the tracers is detected by a gamma camera, which creates images that show the function of the organs or tissues.
Factors Influencing Image Quality
Image quality is a critical aspect of diagnostic imaging. It refers to the clarity and sharpness of the image, which directly impacts the accuracy of diagnosis and treatment planning. Several factors influence image quality, including:
- Contrast: Contrast refers to the difference in brightness between adjacent areas on an image. High contrast means there is a large difference in brightness, making it easier to distinguish between different tissues. Factors that affect contrast include the type of radiation used, the patient’s size and composition, and the technique settings.
- Resolution: Resolution refers to the ability to distinguish between two closely spaced objects on an image. High resolution means that small objects can be clearly seen. Factors that affect resolution include the size of the image receptor, the distance between the source and the patient, and the magnification used.
- Noise: Noise refers to random variations in the image signal that can obscure details. Noise can be caused by factors such as scatter radiation, electronic noise, and patient motion. Noise reduces image quality and can make it difficult to interpret the image.
Techniques for Optimizing Image Quality
Several techniques can be used to optimize image quality, including:
- Proper Positioning: Correct patient positioning is essential for ensuring that the desired anatomy is captured on the image. Incorrect positioning can result in distortion or obscuring of important structures.
- Collimation: Collimation restricts the beam of radiation to the area of interest, reducing scatter radiation and improving image quality. It also reduces the radiation dose to the patient.
- kVp and mAs Selection: kVp (kilovolt peak) controls the energy of the X-ray beam, while mAs (milliampere-seconds) controls the amount of radiation produced. Proper selection of these parameters is crucial for achieving optimal contrast and exposure.
- Grid Use: Grids are used to absorb scatter radiation, which improves image contrast. The use of a grid is often necessary for larger body parts or when using high kVp techniques.
- Image Processing: Digital image processing techniques can be used to enhance image quality by reducing noise, improving contrast, and sharpening edges. These techniques are often applied automatically by the imaging system.
- Patient Preparation: Patient preparation, such as fasting or bowel cleansing, can improve image quality by reducing artifacts and enhancing visibility of specific structures.
Image Artifacts
Image artifacts are any unwanted features on an image that can obscure or distort the true anatomy. Artifacts can be caused by a variety of factors, including:
- Motion: Patient motion during the imaging process can create blurring or distortion on the image. This is a common artifact, especially in children or patients who are unable to hold still.
- Scatter Radiation: Scatter radiation is radiation that has been deflected from its original path and can create a fog-like appearance on the image. This artifact can be reduced by using collimation, grids, and proper technique settings.
- Metal Objects: Metal objects, such as jewelry or surgical implants, can create white streaks or shadows on the image. These artifacts can be minimized by removing metal objects before imaging or using special imaging techniques.
- Air Bubbles: Air bubbles in the patient’s body or in the imaging equipment can create dark areas on the image. This artifact is common in ultrasound imaging.
- Equipment Malfunction: Malfunctions in the imaging equipment can create a variety of artifacts, including lines, streaks, and distortions. Regular equipment maintenance is essential for minimizing artifacts.
Radiographic Positioning and Technique
Radiographic positioning is a critical aspect of radiologic technology. It involves the precise placement of the patient and the x-ray beam to obtain optimal images for diagnosis. Proper positioning ensures that the desired anatomical structures are captured clearly, while minimizing exposure to the patient and the technologist. This chapter will delve into the principles of radiographic positioning, anatomical landmarks used in positioning, different radiographic projections, and their applications.
Principles of Radiographic Positioning
The principles of radiographic positioning guide the technologist in obtaining high-quality images. These principles ensure that the desired anatomical structures are projected clearly on the image receptor, minimizing distortion and maximizing diagnostic information.
- Central Ray Alignment: The central ray of the x-ray beam should be directed through the anatomical structure of interest. This ensures that the structure is positioned in the center of the image receptor, minimizing distortion and maximizing detail.
- Body Position: The patient’s body should be positioned correctly to ensure that the anatomical structure of interest is aligned with the x-ray beam. This involves positioning the patient’s limbs, torso, and head in a specific manner depending on the desired projection.
- Image Receptor Placement: The image receptor should be positioned correctly to capture the desired anatomical structures. This involves aligning the image receptor with the central ray of the x-ray beam and ensuring that it is positioned close enough to the patient to minimize magnification.
- Collimation: The x-ray beam should be collimated to the size of the anatomical structure of interest. This minimizes scatter radiation, improving image quality and reducing patient exposure.
Anatomical Landmarks, Introduction to radiologic technology 8th edition
Anatomical landmarks are essential for radiographic positioning. They serve as reference points to ensure that the patient is positioned correctly and that the central ray of the x-ray beam is directed through the desired anatomical structure.
- Bony Landmarks: These include bony prominences, such as the iliac crest, the acromion process, and the greater trochanter, which are easily palpable and serve as reliable reference points.
- Surface Landmarks: These include external features, such as the midline of the body, the vertebral spinous processes, and the nipple line, which provide visual references for positioning.
Radiographic Projections
Radiographic projections are the different ways in which the x-ray beam is directed through the patient. Each projection provides a unique view of the anatomical structures, allowing for a comprehensive evaluation.
- AP (Anteroposterior): The x-ray beam enters the anterior aspect of the body and exits the posterior aspect.
- PA (Posterioanterior): The x-ray beam enters the posterior aspect of the body and exits the anterior aspect.
- Lateral: The x-ray beam enters the side of the body and exits the opposite side.
- Oblique: The x-ray beam enters the body at an angle, providing a specific view of the anatomical structures.
Radiographic Procedures and Positioning Requirements
The following table summarizes common radiographic procedures and their positioning requirements:
| Procedure | Positioning Requirements |
|---|---|
| Chest X-ray | PA and lateral projections, with the patient standing or sitting upright |
| Abdominal X-ray | AP projection, with the patient supine |
| Pelvis X-ray | AP projection, with the patient supine |
| Skull X-ray | PA and lateral projections, with the patient supine |
| Spine X-ray | AP and lateral projections, with the patient standing or lying prone |
| Extremity X-ray | AP and lateral projections, with the patient standing or lying prone |
Radiographic Equipment and Procedures: Introduction To Radiologic Technology 8th Edition
Radiographic equipment and procedures are essential components of medical imaging, providing valuable diagnostic information for healthcare professionals. Understanding the intricacies of these systems and techniques is crucial for radiologic technologists to ensure safe and effective image acquisition.
Components of a Radiographic System
A typical radiographic system consists of several interconnected components, each playing a crucial role in generating and capturing X-ray images.
- X-ray Tube: The heart of the system, the X-ray tube generates X-rays by accelerating electrons toward a metal target. This process creates a beam of high-energy photons that penetrate the body.
- High-Voltage Generator: This component provides the high voltage necessary to accelerate electrons within the X-ray tube. It controls the voltage and current applied to the tube, influencing the energy and quantity of X-rays produced.
- Control Console: This user interface allows the radiologic technologist to select the technical factors, such as kilovoltage peak (kVp), milliamperage (mA), and exposure time, that determine the quality and quantity of X-rays produced. It also displays essential information, such as the exposure parameters and patient data.
- Collimator: This device shapes the X-ray beam, limiting its size and reducing scatter radiation. It includes a lead diaphragm with adjustable shutters that control the beam’s width and length, ensuring that only the desired area is exposed to radiation.
- Image Receptor: This component captures the X-ray beam after it has passed through the patient’s body. It converts the X-ray energy into a visible image. Common image receptors include film, digital detectors, and fluoroscopic screens.
- Table: The radiographic table provides a stable platform for the patient during the examination. It may be equipped with various features, such as a Bucky tray for image receptor support, a tilting mechanism, and a floating top for easier patient positioning.
Operation and Function of Radiographic Equipment
The operation of a radiographic system involves a series of steps that transform electrical energy into X-ray photons and capture the resulting image.
- Electrical Energy Supply: The process begins with the flow of electrical current from the power supply to the high-voltage generator.
- Electron Generation: Within the X-ray tube, a heated filament emits electrons through thermionic emission. These electrons are then accelerated towards the anode target by the high voltage applied by the generator.
- X-ray Production: As the accelerated electrons collide with the anode target, they release energy in the form of X-ray photons. These photons are emitted in a specific direction, forming the X-ray beam.
- Beam Shaping and Filtration: The X-ray beam is then directed through the collimator, which shapes the beam and reduces scatter radiation. The beam may also pass through filters, such as aluminum, to remove low-energy photons that contribute to patient dose without improving image quality.
- Image Capture: The X-ray beam interacts with the image receptor, producing an image that represents the distribution of X-ray photons that have passed through the patient. This image can be captured on film, stored in a digital format, or viewed directly on a fluoroscopic screen.
Types of Radiographic Procedures
Radiographic procedures can be categorized based on the specific body region or clinical indication.
- General Radiography: This encompasses a wide range of procedures, including chest X-rays, abdominal X-rays, skeletal radiography, and extremity radiography. These procedures utilize conventional X-ray techniques to visualize various anatomical structures.
- Fluoroscopy: This technique uses a continuous X-ray beam to create real-time images on a monitor. It allows for dynamic visualization of moving structures, such as the gastrointestinal tract during a barium swallow or the heart during a cardiac catheterization.
- Mammography: This specialized procedure uses low-dose X-rays to visualize breast tissue. It plays a crucial role in early breast cancer detection and screening.
- Computed Tomography (CT): This advanced imaging technique uses a rotating X-ray source and detectors to create cross-sectional images of the body. It provides detailed anatomical information and is often used for diagnosing a wide range of conditions, including cancer, trauma, and vascular disease.
- Magnetic Resonance Imaging (MRI): This technique uses a strong magnetic field and radio waves to create detailed images of soft tissues and organs. It is particularly useful for imaging the brain, spinal cord, and joints.
Steps Involved in a Typical Radiographic Procedure
A typical radiographic procedure follows a standardized sequence of steps to ensure safety, accuracy, and optimal image quality.
- Patient Preparation: This step involves gathering patient history, explaining the procedure, and ensuring the patient’s comfort and safety. The technologist may also need to remove any metal objects or clothing that could interfere with the image.
- Positioning: The technologist positions the patient correctly to ensure that the desired anatomical structures are captured in the image. Proper positioning is crucial for accurate diagnosis and minimizing radiation exposure.
- Technical Factor Selection: The technologist selects the appropriate technical factors, such as kVp, mA, and exposure time, based on the patient’s size, body part being imaged, and desired image quality. These factors determine the energy and quantity of X-rays produced.
- Exposure: The technologist initiates the exposure, delivering the X-ray beam to the patient. During the exposure, the patient must remain still to avoid motion artifacts.
- Image Processing: After the exposure, the image is processed, either manually using film or digitally using a computer system. This step involves converting the X-ray signal into a visible image.
- Image Evaluation: The technologist reviews the image to ensure that it is technically acceptable and meets diagnostic criteria. This involves checking for proper positioning, exposure, and image quality.
- Image Interpretation: The radiologist, a physician specializing in medical imaging, interprets the images to identify any abnormalities or disease processes.
Radiation Safety and Protection
Radiation safety and protection are paramount in radiologic technology. It is crucial to understand the principles and practices that minimize radiation exposure to patients, personnel, and the environment.
Potential Risks Associated with Radiation Exposure
Exposure to ionizing radiation can have detrimental effects on living organisms. The severity of these effects depends on the amount of radiation absorbed, the type of radiation, and the sensitivity of the tissues exposed.
- Deterministic effects: These effects are directly related to the dose of radiation received. They are characterized by a threshold dose, meaning that they occur only after a certain amount of radiation is absorbed. Examples include skin burns, radiation sickness, and cataracts.
- Stochastic effects: These effects are probabilistic, meaning that the probability of their occurrence increases with the dose of radiation received. There is no threshold dose for these effects. Examples include cancer and genetic mutations.
Methods Used to Minimize Radiation Exposure
Radiologic technologists are responsible for minimizing radiation exposure to patients and themselves. This is achieved through various methods:
- Time: Reducing the duration of radiation exposure minimizes the total dose received. This can be achieved by using efficient techniques and limiting the time spent in the radiation field.
- Distance: The intensity of radiation decreases rapidly with distance from the source. Increasing the distance between the source and the person being exposed reduces the dose received. This is often accomplished through the use of lead shields or by positioning the technologist at a safe distance during procedures.
- Shielding: Lead aprons, gloves, and thyroid shields are commonly used to absorb radiation and protect personnel. Lead-lined walls and barriers also help to reduce radiation exposure in the radiology department.
- Collimation: Restricting the X-ray beam to the area of interest reduces the amount of tissue exposed. This helps to minimize the radiation dose to surrounding tissues and organs.
- Technique optimization: Selecting appropriate exposure factors, such as kilovoltage peak (kVp) and milliampere-seconds (mAs), ensures that adequate images are obtained while minimizing radiation dose.
- Image Receptor Selection: Using digital detectors, which are more sensitive to radiation than traditional film, allows for lower radiation doses to be used.
Radiation Safety Guidelines for Radiographic Procedures
| Procedure | Radiation Safety Guidelines |
|---|---|
| Chest X-ray | – Use appropriate collimation to minimize the exposure field. – Position the patient correctly to minimize the need for repeat exposures. – Use a high-frequency generator to reduce the exposure time. – Ensure the patient is properly shielded with lead aprons or gowns. |
| Abdominal X-ray | – Use appropriate collimation to minimize the exposure field. – Position the patient correctly to minimize the need for repeat exposures. – Use a high-frequency generator to reduce the exposure time. – Ensure the patient is properly shielded with lead aprons or gowns. – Consider using a gonad shield to protect the reproductive organs. |
| Pelvic X-ray | – Use appropriate collimation to minimize the exposure field. – Position the patient correctly to minimize the need for repeat exposures. – Use a high-frequency generator to reduce the exposure time. – Ensure the patient is properly shielded with lead aprons or gowns. – Consider using a gonad shield to protect the reproductive organs. |
| Extremity X-ray | – Use appropriate collimation to minimize the exposure field. – Position the patient correctly to minimize the need for repeat exposures. – Use a high-frequency generator to reduce the exposure time. – Ensure the patient is properly shielded with lead aprons or gowns. – Consider using a lead shield to protect the opposite extremity. |
Quality Assurance and Control
Quality assurance (QA) is an essential component of radiologic imaging, ensuring the consistent production of high-quality images for accurate diagnosis and treatment planning. It involves a systematic process of monitoring and evaluating all aspects of the imaging process to identify and correct any potential problems that could affect image quality.
Methods of Quality Control
Quality control (QC) methods are implemented to ensure the accuracy and reliability of radiographic procedures. These methods are designed to monitor and evaluate specific aspects of the imaging process, such as equipment performance, image processing, and personnel proficiency.
- Equipment Performance Evaluation: Regular testing and calibration of imaging equipment are crucial to ensure optimal performance. This includes evaluating factors like x-ray generator output, collimator accuracy, and image receptor characteristics.
- Image Processing Evaluation: The quality of image processing techniques, such as digital image processing and film development, directly impacts image quality. QC measures involve evaluating factors like contrast, brightness, and resolution.
- Personnel Proficiency Evaluation: Radiologic technologists play a vital role in maintaining image quality. Regular training, competency assessments, and proficiency evaluations are crucial to ensure their skills and knowledge are up to date.
- Image Analysis and Interpretation: Reviewing and evaluating images for technical quality and diagnostic information is an essential aspect of QC. This involves assessing factors like image sharpness, contrast, and the presence of artifacts.
Role of the Radiologic Technologist
Radiologic technologists are directly involved in maintaining quality assurance. They play a crucial role in:
- Performing QC procedures: Technologists are responsible for conducting routine equipment checks, calibrations, and image analysis as part of the overall QC program.
- Following established protocols: Adhering to established imaging protocols, including positioning, technique, and image processing, is essential for consistent image quality.
- Reporting any deviations: Technologists are responsible for identifying and reporting any deviations from established protocols or equipment malfunctions that could impact image quality.
- Participating in continuing education: Staying updated on the latest technologies, techniques, and QC procedures is essential for maintaining proficiency and contributing to QA.
Quality Assurance Indicators
QA indicators are specific measures used to monitor and evaluate the effectiveness of the QA program. These indicators provide valuable insights into the overall quality of radiographic images and the effectiveness of the imaging process.
- Image Rejects: The percentage of images rejected due to technical factors, such as poor positioning, inadequate exposure, or artifacts, can indicate potential issues with the imaging process.
- Repeat Rates: The number of repeated images due to technical errors provides valuable information about the consistency of the imaging process and the effectiveness of QC measures.
- Patient Dose: Monitoring patient radiation dose levels helps ensure that exposure levels are minimized while maintaining diagnostic image quality.
- Equipment Downtime: Tracking the frequency and duration of equipment malfunctions can identify potential problems that require attention and maintenance.
- Personnel Errors: Monitoring the occurrence of personnel errors, such as incorrect positioning or technique, can help identify areas for improvement in training and competency.
Interpretation of Quality Assurance Indicators
The interpretation of QA indicators is crucial for identifying areas where improvements are needed. For example, a high image reject rate may indicate a need for additional training or equipment calibration. Similarly, a high repeat rate may suggest that specific procedures or protocols require review and adjustment. By carefully analyzing QA indicators, healthcare facilities can identify potential problems and implement corrective actions to ensure consistent image quality and patient safety.
Professional Development and Ethics
The field of radiologic technology is constantly evolving, with new technologies and advancements emerging regularly. To remain competent and provide high-quality patient care, radiologic technologists must prioritize professional development. This includes staying abreast of the latest advancements, refining their skills, and upholding ethical standards.
Continuing Education
Continuing education plays a crucial role in ensuring that radiologic technologists remain up-to-date with the latest developments in the field. It helps them adapt to new technologies, improve their diagnostic skills, and maintain their professional competency.
- Professional Organizations: Organizations like the American Society of Radiologic Technologists (ASRT) and the American Registry of Radiologic Technologists (ARRT) offer a wide range of continuing education courses and workshops. These courses cover various topics, including new imaging modalities, radiation safety protocols, and patient care techniques.
- Online Resources: Online platforms provide convenient access to a plethora of continuing education resources, including webinars, articles, and interactive modules. This allows technologists to learn at their own pace and schedule.
- Conferences and Symposia: Attending conferences and symposia provides a platform for networking with colleagues, sharing best practices, and learning about cutting-edge research and advancements in the field.
Professional Organizations and Certifications
Professional organizations play a vital role in supporting radiologic technologists by providing resources, advocating for their interests, and setting standards for the profession.
- American Society of Radiologic Technologists (ASRT): The ASRT is a professional organization dedicated to advancing the profession of radiologic technology. It offers a wide range of resources, including continuing education programs, advocacy efforts, and publications.
- American Registry of Radiologic Technologists (ARRT): The ARRT is a credentialing organization that offers certification exams for various radiologic technology specialties. Passing these exams demonstrates competency and allows technologists to practice legally in many states.
- Other Organizations: Other organizations, such as the Association of Educators in Imaging and Radiologic Sciences (AEIRS), the Society of Diagnostic Medical Sonography (SDMS), and the American College of Radiology (ACR), also play important roles in supporting the field.
Ethical Principles
Ethical principles guide radiologic technologists in their practice, ensuring patient safety, privacy, and well-being. These principles are based on the core values of honesty, integrity, and respect.
- Beneficence: This principle emphasizes the obligation to act in the best interests of the patient. Radiologic technologists should always strive to provide safe and effective care.
- Non-maleficence: This principle requires technologists to avoid causing harm to patients. They must use appropriate techniques and follow safety protocols to minimize the risk of radiation exposure or other complications.
- Autonomy: This principle recognizes the patient’s right to make decisions about their own healthcare. Technologists must respect patient choices and ensure they are informed about procedures and risks.
- Confidentiality: This principle requires technologists to maintain patient confidentiality. They must protect patient information and only share it with authorized personnel.
Ethical Dilemmas
Radiologic technologists may face ethical dilemmas in their practice, requiring them to carefully consider the principles involved and make informed decisions.
- Conflicting Patient Wishes: A patient may refuse a procedure, even if it is medically necessary. Technologists must balance their obligation to provide care with the patient’s right to autonomy.
- Radiation Safety Concerns: Technologists may need to weigh the benefits of a procedure against the potential risks of radiation exposure, particularly for pregnant patients or children.
- Professional Boundaries: Maintaining professional boundaries with patients is essential. Technologists must avoid inappropriate relationships or disclosures of personal information.
Conclusion
Whether you’re a student aspiring to become a radiologic technologist or a seasoned professional seeking to enhance your knowledge and skills, Introduction to Radiologic Technology 8th Edition is an invaluable resource. Its comprehensive coverage, practical approach, and emphasis on ethical practice make it the perfect companion for anyone interested in this essential healthcare profession. As you navigate the ever-evolving landscape of radiologic technology, this book will serve as a trusted guide, empowering you to make informed decisions and provide exceptional patient care.
Understanding the intricacies of radiologic technology, as outlined in the 8th edition of the textbook, is crucial for aspiring professionals. This field, however, is not isolated from broader technological advancements. The emergence of renewable energy sources, like those offered by jznee renewable energy technology , has a direct impact on the medical imaging industry.
The transition towards eco-friendly practices extends to medical facilities, necessitating a comprehensive understanding of how these technologies intersect with radiologic procedures.