Electroneurodiagnostic Technology: A Window into the Brain
Electroneurodiagnostic technology, a powerful tool in healthcare, allows medical professionals to peek into the intricate workings of the brain. This technology uses non-invasive methods to record and analyze the electrical […]
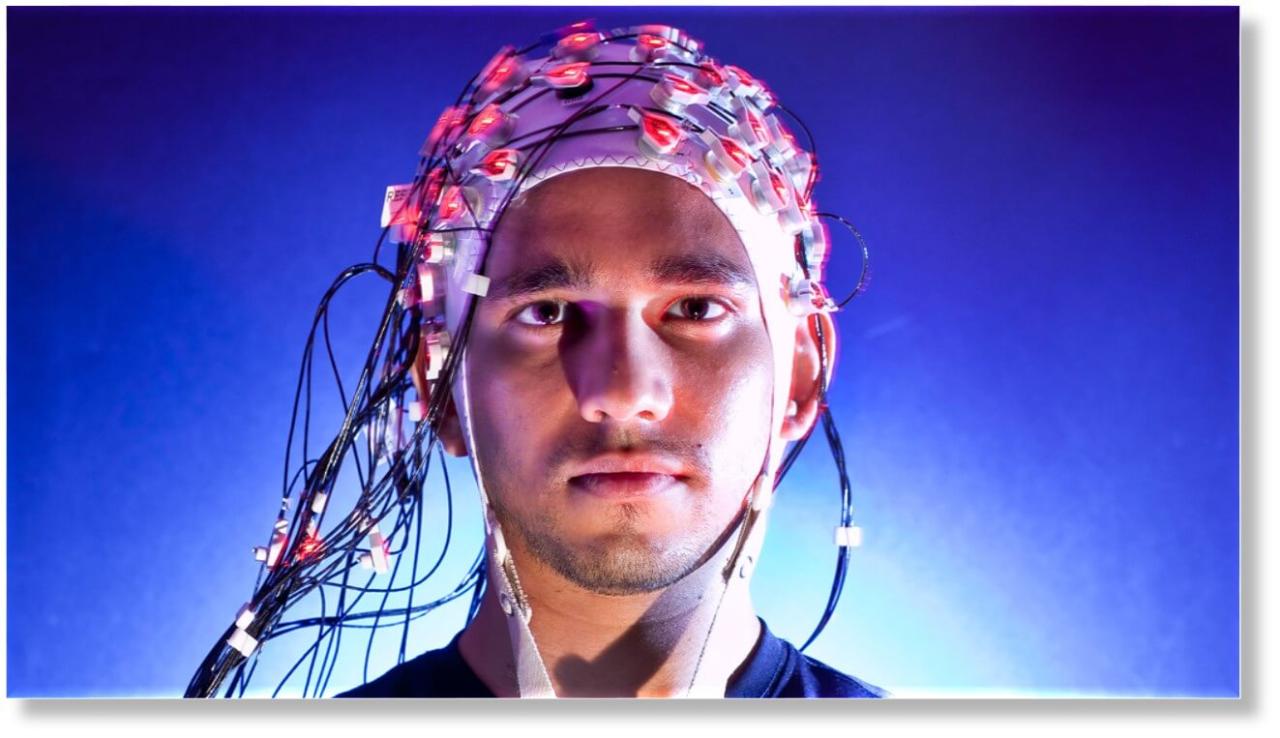
Electroneurodiagnostic technology, a powerful tool in healthcare, allows medical professionals to peek into the intricate workings of the brain. This technology uses non-invasive methods to record and analyze the electrical activity of the nervous system, providing valuable insights into brain function and dysfunction.
From its humble beginnings in the early 20th century, electroneurodiagnostic technology has evolved significantly, becoming a cornerstone of diagnosis and treatment for a wide range of neurological conditions. This field encompasses various techniques, including electroencephalography (EEG), electromyography (EMG), and nerve conduction studies, each offering unique perspectives on the brain’s intricate electrical symphony.
Introduction to Electroneurodiagnostic Technology
Electroneurodiagnostic (END) technology is a specialized field of healthcare that uses non-invasive techniques to record and analyze the electrical activity of the nervous system. END plays a crucial role in diagnosing, monitoring, and managing various neurological conditions.
History and Evolution of END Technology
The history of END technology dates back to the late 19th century, with the invention of the electroencephalograph (EEG) by Hans Berger. The EEG allowed for the recording and visualization of brainwaves, paving the way for the diagnosis of epilepsy and other neurological disorders. Over the years, END technology has evolved significantly, with the development of new techniques and advancements in instrumentation.
Key Applications and Benefits of END Technology
END technology has a wide range of applications in healthcare, including:
- Diagnosis of Neurological Disorders: END tests are essential for diagnosing a variety of neurological disorders, such as epilepsy, stroke, brain tumors, and sleep disorders. For example, EEG recordings can help identify abnormal brain activity patterns characteristic of epilepsy.
- Monitoring Neurological Function: END techniques can be used to monitor neurological function in patients with existing conditions, such as coma or brain injury. For instance, continuous EEG monitoring can detect changes in brain activity that may indicate worsening neurological status.
- Neuromuscular Disorders: END technology is also used to diagnose and monitor neuromuscular disorders, such as myasthenia gravis and amyotrophic lateral sclerosis (ALS). Electromyography (EMG) and nerve conduction studies are essential tools in these evaluations.
- Research and Development: END technology plays a vital role in research and development related to the nervous system. Researchers use END techniques to study brain function, cognitive processes, and the effects of various medications and therapies.
Types of Electroneurodiagnostic Tests

Electroneurodiagnostic (END) technology encompasses a range of tests that utilize electrical signals to assess the function of the nervous system. These tests play a crucial role in diagnosing and monitoring neurological conditions, aiding in the development of effective treatment plans.
Electroencephalography (EEG)
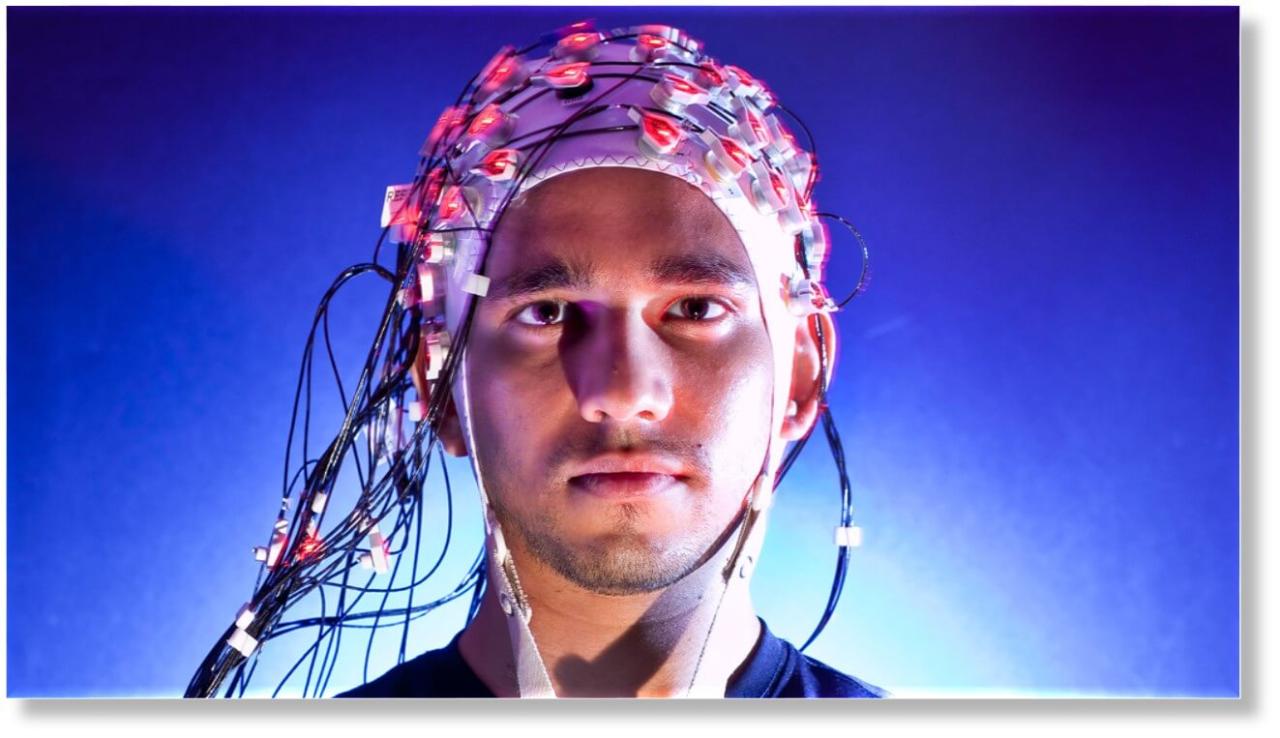
EEG is a non-invasive test that records the electrical activity of the brain through electrodes placed on the scalp. It is commonly used to diagnose conditions such as epilepsy, sleep disorders, brain tumors, and encephalopathies.
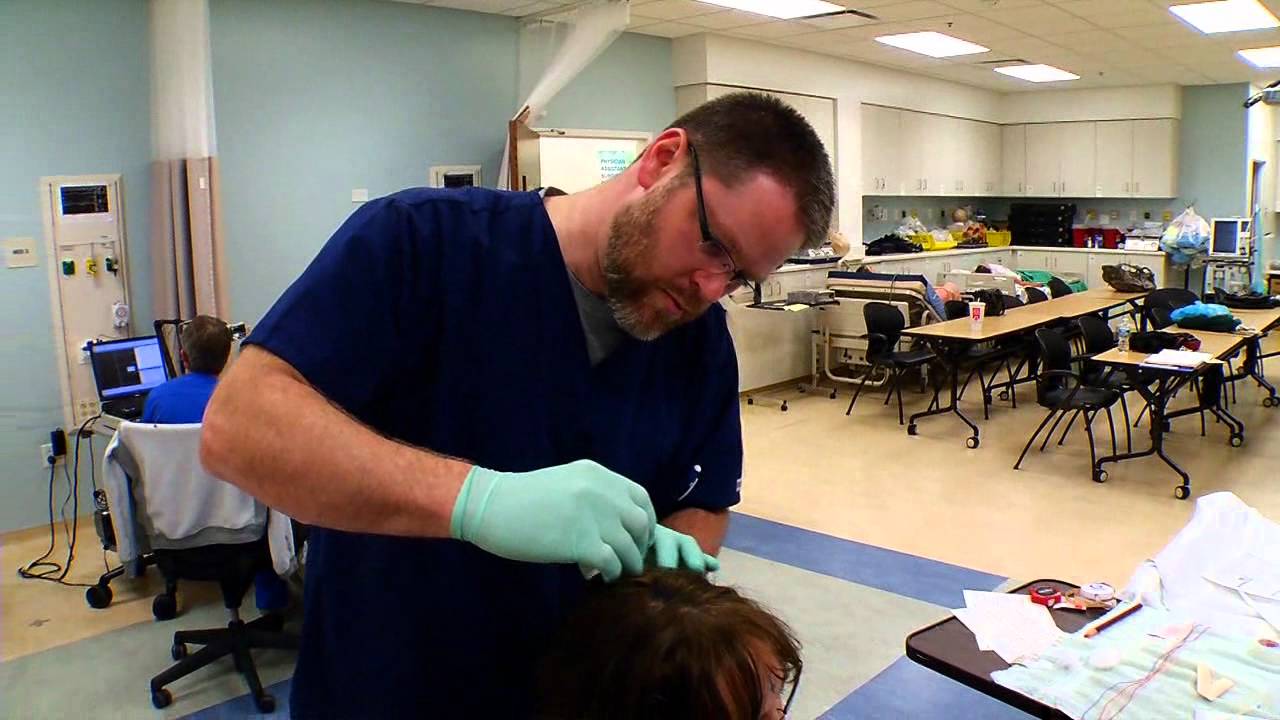
The procedure involves placing a series of electrodes on the scalp, usually with a conductive paste to ensure a good electrical connection. The electrodes pick up electrical signals from the brain, which are amplified and displayed on a computer screen. The resulting waveforms are analyzed by a trained technician or neurologist, who can identify abnormalities in brain activity.
EEG is often used to:
- Identify the type and location of seizures in patients with epilepsy.
- Diagnose sleep disorders, such as insomnia, narcolepsy, and sleep apnea.
- Monitor brain activity during surgery or anesthesia.
- Evaluate the severity of a coma or brain injury.
- Detect brain tumors or other structural abnormalities.
Electromyography (EMG)
EMG is a diagnostic test that measures the electrical activity of muscles. It is used to assess the health of the nerves and muscles, and to diagnose conditions such as nerve damage, muscle disorders, and spinal cord injuries.
The procedure involves inserting small needle electrodes into the muscles. The electrodes pick up electrical signals from the muscles, which are amplified and displayed on a computer screen. The resulting waveforms are analyzed by a trained technician or neurologist, who can identify abnormalities in muscle activity.
EMG is often used to:
- Diagnose nerve damage, such as carpal tunnel syndrome, sciatica, and peripheral neuropathy.
- Evaluate muscle disorders, such as muscular dystrophy and myasthenia gravis.
- Assess the severity of spinal cord injuries.
- Monitor the effectiveness of treatment for neurological conditions.
Nerve Conduction Studies (NCS), Electroneurodiagnostic technology
NCS are a series of tests that measure the speed and amplitude of electrical signals traveling along nerves. They are used to diagnose nerve damage, determine the severity of nerve injury, and monitor the effectiveness of treatment.
The procedure involves placing electrodes on the skin over the nerve being tested. A small electrical stimulus is applied to the nerve, and the time it takes for the signal to reach the next electrode is measured. This information is used to calculate the nerve conduction velocity, which is a measure of how fast the nerve is conducting electrical signals.
NCS are often used to:
- Diagnose nerve damage, such as carpal tunnel syndrome, sciatica, and peripheral neuropathy.
- Determine the severity of nerve injury.
- Monitor the effectiveness of treatment for nerve damage.
Evoked Potentials (EP)
EP are a group of tests that measure the electrical activity of the brain in response to sensory stimulation. They are used to diagnose a variety of neurological conditions, including multiple sclerosis, brain tumors, and spinal cord injuries.
The procedure involves applying a sensory stimulus, such as light, sound, or touch, to the patient. The electrical activity of the brain in response to the stimulus is then recorded using electrodes placed on the scalp. The resulting waveforms are analyzed by a trained technician or neurologist, who can identify abnormalities in brain activity.
EP are often used to:
- Diagnose multiple sclerosis, a disease that affects the central nervous system.
- Evaluate the severity of brain tumors and spinal cord injuries.
- Monitor the effectiveness of treatment for neurological conditions.
Polysomnography (PSG)
PSG is a comprehensive sleep study that records various physiological parameters during sleep, including brain activity (EEG), eye movements (EOG), muscle activity (EMG), and breathing patterns. It is used to diagnose and treat sleep disorders, such as insomnia, sleep apnea, and narcolepsy.
The procedure involves spending a night in a sleep lab, where a technician monitors the patient’s sleep patterns using various sensors and electrodes. The data collected during the sleep study is then analyzed by a sleep specialist, who can identify any abnormalities in sleep patterns.
PSG is often used to:
- Diagnose sleep apnea, a condition where breathing repeatedly stops and starts during sleep.
- Identify other sleep disorders, such as insomnia, narcolepsy, and restless legs syndrome.
- Evaluate the effectiveness of treatment for sleep disorders.
Equipment and Technology Used
Electroneurodiagnostic (END) technology relies on a variety of specialized equipment to capture, amplify, and analyze electrical signals generated by the nervous system. These instruments are essential for accurately diagnosing and monitoring neurological conditions.
Electroencephalography (EEG) Equipment
EEG equipment is used to record the electrical activity of the brain. The main components include:
- Electrodes: Small, metal discs or pads attached to the scalp using conductive paste or gel. They detect the electrical signals from the brain and transmit them to the amplifier.
- Amplifier: A device that amplifies the weak electrical signals from the electrodes, making them visible on the EEG recording.
- Recording Device: A computer or specialized machine that records the amplified EEG signals, often in the form of a waveform on a screen or printed paper.
- Software: Modern EEG systems use software to analyze the recorded signals, identify abnormalities, and generate reports.
Evoked Potentials (EP) Equipment
EP equipment is used to measure the brain’s response to specific stimuli, such as visual, auditory, or tactile inputs.
- Stimulators: Devices that deliver the specific stimuli to the patient, such as lights, sounds, or vibrations.
- Electrodes: Similar to EEG electrodes, they are placed on the scalp to detect the brain’s response to the stimuli.
- Amplifier and Recording Device: Similar to EEG equipment, these components amplify and record the electrical signals related to the evoked potentials.
- Averaging System: A software component that averages multiple responses to the stimuli to isolate the specific brain response from background noise.
Electromyography (EMG) Equipment
EMG equipment is used to measure the electrical activity of muscles.
- Electrodes: Needle electrodes are inserted into the muscle to record the electrical signals produced by muscle fibers.
- Amplifier: Similar to EEG and EP equipment, it amplifies the muscle signals.
- Recording Device: A computer or specialized machine records the EMG signals, often displaying them as waveforms on a screen.
- Stimulator: Some EMG tests use a stimulator to deliver electrical impulses to nerves to assess their ability to transmit signals to muscles.
Nerve Conduction Studies (NCS) Equipment
NCS equipment measures the speed and amplitude of electrical signals traveling along nerves.
- Stimulator: Delivers electrical impulses to a nerve to initiate a signal.
- Electrodes: Recording electrodes are placed over the nerve at different locations to detect the signal as it travels along the nerve.
- Amplifier and Recording Device: Similar to other END equipment, these components amplify and record the nerve signals.
- Software: Specialized software analyzes the nerve conduction velocity and amplitude to assess nerve function.
Advancements and Emerging Technologies
The field of END technology is constantly evolving, with new advancements and emerging technologies improving diagnostic accuracy and patient care. Some notable examples include:
- High-Density EEG (HD-EEG): This technique uses a higher number of electrodes, providing a more detailed picture of brain activity. HD-EEG is particularly useful for localizing seizure activity.
- Quantitative EEG (QEEG): QEEG uses advanced algorithms to analyze EEG data, providing quantitative measures of brain function that can help diagnose and monitor neurological disorders.
- Brain-Computer Interfaces (BCIs): BCIs are being developed to allow communication and control of devices using brain signals. This technology has the potential to improve the lives of individuals with severe disabilities.
- Portable and Wearable Devices: Advances in miniaturization and wireless technology have led to the development of portable and wearable EEG devices, allowing for continuous monitoring of brain activity outside of a clinical setting.
Interpretation and Analysis of Results
The interpretation and analysis of electroneurodiagnostic test results are crucial for accurate diagnosis and treatment planning. These tests provide valuable insights into the electrical activity of the brain and nervous system, allowing healthcare professionals to identify abnormalities and understand their underlying causes.
The Role of Qualified Professionals
The interpretation of electroneurodiagnostic test results requires specialized knowledge and expertise. Qualified professionals, such as neurologists, electroencephalographers (EEGs), and other trained personnel, are responsible for analyzing the data and drawing conclusions based on their findings. These professionals have extensive training in interpreting the complex patterns of electrical activity, recognizing variations from normal, and correlating them with clinical presentations.
Typical Findings and Their Clinical Significance
- Abnormal EEG Patterns:
- Epileptiform Activity: The presence of spikes, sharp waves, or other characteristic patterns in the EEG suggests an increased risk of seizures or other neurological disorders.
- Slow Wave Activity: An abundance of slow waves in the EEG can indicate brain damage, metabolic disorders, or other conditions affecting brain function.
- Asymmetry: Differences in electrical activity between the two hemispheres of the brain can point to focal lesions, stroke, or other neurological events.
- Abnormal Nerve Conduction Studies:
- Slowed Nerve Conduction Velocity: Reduced nerve conduction velocity can indicate nerve damage, compression, or other conditions affecting nerve function.
- Abnormal Amplitude: Decreased or absent amplitude of nerve signals can indicate nerve damage, muscle disorders, or other conditions affecting the neuromuscular junction.
- Prolonged Latency: Increased latency of nerve signals can suggest nerve damage, demyelination, or other conditions affecting nerve conduction.
- Abnormal Evoked Potentials:
- Delayed Latency: Prolonged latency of evoked potentials can indicate damage to the sensory pathways or other neurological conditions affecting sensory processing.
- Reduced Amplitude: Decreased amplitude of evoked potentials can indicate damage to the sensory pathways or other neurological conditions affecting sensory processing.
- Abnormal Waveform: Distortions in the waveform of evoked potentials can indicate abnormalities in the central nervous system or other neurological conditions affecting sensory processing.
Clinical Applications and Benefits
Electroneurodiagnostic technology plays a vital role in diagnosing, treating, and managing a wide range of neurological conditions. By providing insights into the electrical activity of the brain and nervous system, these tests help healthcare professionals understand the underlying causes of neurological disorders and make informed decisions about patient care.
Diagnosis of Neurological Disorders
Electroneurodiagnostic tests are essential for the diagnosis of various neurological conditions, including:
- Epilepsy: Electroencephalography (EEG) is the gold standard for diagnosing epilepsy. It helps identify seizure activity and determine the type and location of seizures, guiding treatment decisions.
- Brain tumors: EEG can detect abnormal electrical activity in the brain caused by tumors, helping to pinpoint their location and size.
- Stroke: Electroencephalogram (EEG) can help identify brain damage caused by stroke, providing information about the severity and location of the stroke.
- Sleep disorders: Polysomnography (PSG), a type of sleep study, is used to diagnose sleep disorders such as insomnia, sleep apnea, and restless leg syndrome.
- Dementia: EEG can help distinguish between different types of dementia, such as Alzheimer’s disease and vascular dementia, by identifying specific patterns of brain activity.
- Head injuries: EEG can detect brain damage caused by head injuries, helping to assess the severity of the injury and guide treatment.
- Multiple sclerosis (MS): Evoked potentials, a type of neurophysiological test, can help diagnose MS by measuring the speed at which nerve signals travel along the spinal cord and brain.
Treatment Planning and Management
Electroneurodiagnostic tests are crucial for planning and managing treatment for neurological disorders.
- Epilepsy: EEG helps determine the best medication and dosage for treating seizures, and can also be used to monitor the effectiveness of treatment.
- Brain tumors: EEG can help monitor the response to treatment, such as surgery or radiation therapy, and detect any changes in brain activity that may indicate tumor growth or recurrence.
- Stroke: EEG can help guide the treatment of stroke, such as the use of clot-busting drugs or surgery.
- Sleep disorders: PSG can help determine the best treatment for sleep disorders, such as continuous positive airway pressure (CPAP) for sleep apnea.
- Dementia: EEG can help monitor the progression of dementia and assess the effectiveness of treatment.
- Head injuries: EEG can help monitor the recovery from head injuries and identify any complications that may arise.
- Multiple sclerosis (MS): Evoked potentials can help monitor the progression of MS and assess the effectiveness of treatment.
Real-World Examples of Improved Patient Outcomes
Electroneurodiagnostic technology has significantly improved patient outcomes in numerous cases.
- Epilepsy: EEG has helped identify and treat seizures in patients who were previously misdiagnosed or untreated, leading to improved quality of life and reduced risk of injury.
- Brain tumors: EEG has helped guide surgical interventions for brain tumors, leading to more accurate tumor removal and better outcomes for patients.
- Stroke: EEG has helped identify and treat stroke patients more effectively, leading to reduced disability and improved chances of recovery.
- Sleep disorders: PSG has helped diagnose and treat sleep disorders such as sleep apnea, leading to improved sleep quality and reduced daytime fatigue.
- Dementia: EEG has helped distinguish between different types of dementia, allowing for more targeted treatment and support for patients and their families.
- Head injuries: EEG has helped monitor the recovery from head injuries, identifying any complications and guiding treatment decisions.
- Multiple sclerosis (MS): Evoked potentials have helped diagnose and monitor MS, leading to earlier intervention and improved management of the disease.
Ethical Considerations and Safety
Electroneurodiagnostic technology plays a crucial role in diagnosing and monitoring neurological disorders. However, its application raises ethical considerations and necessitates robust safety protocols to ensure patient well-being.
Ethical Considerations
Ethical considerations in electroneurodiagnostic technology focus on patient autonomy, confidentiality, and the responsible use of sensitive information.
- Informed Consent: Patients must be fully informed about the procedures, potential risks, and benefits of electroneurodiagnostic tests before providing consent. The explanation should be clear, concise, and tailored to their understanding.
- Confidentiality: Electroneurodiagnostic tests generate sensitive information about a patient’s neurological function. Maintaining confidentiality is paramount. Access to patient records should be restricted to authorized personnel, and data should be securely stored and handled in compliance with relevant regulations.
- Data Security: The increasing use of digital technology in electroneurodiagnostic procedures necessitates robust data security measures. Measures should be in place to prevent unauthorized access, data breaches, and misuse of patient information.
- Competence and Expertise: Electroneurodiagnostic testing requires specialized knowledge and skills. Only qualified and experienced professionals should perform these procedures to ensure accurate results and minimize the risk of complications.
Safety Protocols and Procedures
Ensuring patient safety is paramount in electroneurodiagnostic procedures.
- Equipment Safety: All equipment used in electroneurodiagnostic procedures must be properly maintained, calibrated, and tested regularly to ensure optimal functionality and minimize the risk of malfunctions.
- Patient Preparation: Before the test, patients should be informed about any necessary preparations, such as avoiding caffeine or alcohol, and any potential discomfort they might experience.
- Electrode Placement: Electrode placement is crucial for accurate signal recording. Proper techniques and standardized guidelines should be followed to minimize discomfort and potential skin irritation.
- Environmental Safety: The testing environment should be quiet, comfortable, and free from distractions. This helps minimize noise artifacts and ensure optimal recording conditions.
- Monitoring and Supervision: During the test, patients should be closely monitored for any adverse reactions, discomfort, or changes in their condition. The technologist should be trained to identify and respond to potential complications.
Potential Complications and Management Strategies
While electroneurodiagnostic procedures are generally safe, potential complications can occur.
- Skin Irritation: Electrode placement can sometimes cause mild skin irritation or redness. Using hypoallergenic adhesives and proper skin preparation can minimize this risk.
- Seizures: In rare cases, electroneurodiagnostic procedures can trigger seizures, particularly in individuals with epilepsy. This risk is minimized by careful patient selection and monitoring during the test.
- Allergic Reactions: Some patients may experience allergic reactions to the adhesive used for electrode placement. Using hypoallergenic adhesives and pre-testing for sensitivities can mitigate this risk.
- Discomfort: Electrode placement and stimulation can cause discomfort or pain in some individuals. Using proper techniques, adjusting electrode placement, and providing pain relief measures can help manage discomfort.
Concluding Remarks
Electroneurodiagnostic technology continues to evolve, with advancements in equipment and analysis techniques constantly pushing the boundaries of our understanding of the brain. As this field continues to grow, it holds the promise of even greater insights into the mysteries of the nervous system, leading to improved diagnoses, personalized treatment plans, and ultimately, enhanced patient outcomes.
Electroneurodiagnostic technology plays a crucial role in diagnosing and monitoring neurological conditions. This field relies heavily on advanced equipment and software, requiring skilled professionals who can operate and interpret the data. For those interested in pursuing a career in this area, a technology fellow program can provide valuable hands-on experience and mentorship.
By gaining expertise in electroneurodiagnostic technology, fellows contribute to the advancement of patient care and contribute to the development of new diagnostic tools.